infections -irritations and injections
 I get many questions about infections or even abcesses. Mostly people blame the Underground Lab, posting the product was not sterile etc. In reality its better first to check on Google if you can find more cases of infection. Because a batch is in most cases much bigger than 1 vial. Most UG labs manufactur a kilo of API (raw powder). A batch of 250 mg/ml wil therefore be around 400 pcs.
I get many questions about infections or even abcesses. Mostly people blame the Underground Lab, posting the product was not sterile etc. In reality its better first to check on Google if you can find more cases of infection. Because a batch is in most cases much bigger than 1 vial. Most UG labs manufactur a kilo of API (raw powder). A batch of 250 mg/ml wil therefore be around 400 pcs.
The culprit in most cases is a lack of knowledge. I’ve seen many times that bodybuilders injected each other or themselves. They clean the injectionspot with alcohol (betadine is much and much better) and immidiatly pierce the skin. After the injection they pull up their pants and boxer. They mostly forget that they have created an open wound, a small one but bacteria are small too.
Once you have desinfected the skin you should wait some time to allow the bacteria to die, before you pierce the skin.
You should also desinfect the top of the vial you keep in the basement or fridge. And use clean needles and syringes. Wash your hands carefully also.
Here you can read how an extremely knowledgeble competing bodybuilder managed to contaminate his vial. When I showed him the analytical reports he realised how lucky he had been for quite some time. He was injecting so much for such a long time that he had become careless about sterility.
//juicedmuscle.com/jmblog/content/bacterial-contamination-10-ml-vial
******************************************************************************************************************
You will notice in an infection (usually) within 3 days and it will be red, sensitive to the touch and will seem to spread. Irritiation for the for first days will be very much the same so it can be stressful during that time to determine what is what.
First off its always a good idea to have some antibiotics handy just in case. Even with pharmaceutical gear from compounding pharmacies you can still get infections from a various amount of reasons. You mentioned injecting in the tricep. Thats a great area to site inject but can be tricky. you need to make sure you flex the tricep fully and find the peak. Watch it carefully as you relax the arm (should be bent 90 degrees not straight) and inject in the center of the meaty portion of the peak. It is very easy to be off center or to hit the outside head where there is not much space and the subsequent expansion of the muscle accompanied with the 2 propionate esters in sustanon to cause some pretty uncomfortable irritation. If the site has not been swabbed with alcohol and a frest needle used that can place bacteria in the injection site.
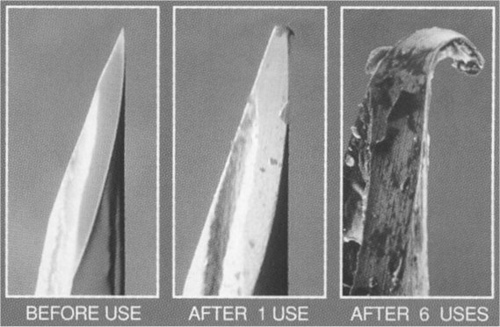
One big pitfall I see every day with people is they will get a syringe with a needle already attached. They will use that needle to draw out the gear and then use the same needle to inject. This is a very unsafe and incorrect practice. You should use something like an 18g loading needle to load the syringe and then switch the needle with a completely fresh needle for the injection. When the same needle is used the hard rubber stopper dulls and bends the tip of the needle up to 60%. This causes irritation, scar tissue and discomofort which alone can cause inflammation or infection.
My suggestion is purchase the syringe/needle combos with the 18g needle already in place. Then purchase seperate boxes of individual needles for the injections themselves. You will notice a night and day difference, infection and irritation will be pretty much eliminated as long as you are using proper sanitation techniques and legitimate gear.
Discussion
Universal symbols frequently associated with physicians are the stethoscope and the hypodermic syringe and needle. Early in the 19th century, scientists were able to purify and isolate active ingredients of several drugs, which would allow small quantities of the drugs to be administered to patients to get desired effects. Subsequently, physicians began searching for ways to administer these drugs so that the medications could be quickly absorbed into the bloodstream and not be altered or destroyed by digestive juices of the patients.[1] Thus, the idea of administering drugs through the skin was conceived. As early as 1809, the French physiologist, Francois Magendie, coated wooden slivers with a drug and pushed it through the skin of his patients. The technique was successful, but unfortunately his patients died. The drug he administered was later found to be strychnine.[1] The administration of medications by hypodermic injection, a term originating from two Greek words that mean "under the skin," was introduced by a Scottish physician, Alexander Wood, in 1853. He attempted to relieve the pain of patients with neuralgia by placing medication next to the involved nerves.[1] The complete history of the development of hypodermic injection of medication can be found in the references.[1]
IM Injection Complications
The first reported complication of the hypodermic injection of medication was reported by Dr. Charles Hunter, a London surgeon, in 1865.[2] Two of his patients who received multiple morphine injections subsequently developed subcutaneous abscesses at the injection sites. At the time of his report, there was no sterilization of medications, syringes, or needles. It was not until 1867, twelve years after Dr. Wood introduced hypodermic injection of medication, that Dr. Joseph Lister published his work on surgical antisepsis and germs. Strangely, complications of hypodermic injection must have been exceedingly uncommon because Dr. Hunter, whose patients developed the first reported complications, said that "if the site of the injection was continually varied and the puncture was made with care and celerity, there was no fear of abscess or diffuse inflammation."[2]
By 1880, complications from the technique were beginning to be recognized. In that year, Dr. H. H. Kane of the United States surveyed physicians worldwide and found all were seeing patients who suffered infectious complications due to hypodermic injection of medications. It was not until 1885 that the complications of this widely practiced procedure were acknowledged by the medical profession.[1]
Today, the incidence of developing a complication from IM injections ranges from 0.4 percent3 to 19.3 percent[4] of patients receiving the IM injection of a medication. The complications that can occur following this procedure are numerous, and some are surprising (Table 1). It has been suggested that most of the problems stemming from the procedure are related to local trauma of the injection itself or the irritating properties of the drug.[3] Others suggest that inadequate training in the proper injection technique is responsible for many of the complications.[5] In some cases, the true etiology of the problem is not immediately apparent.
Leakage. Leakage or seeping of the injected solution from the injection site after the needle is removed seems to be an insignificant problem but can result in erratic absorption of the medication and loss of the expected dose of the medication. This usually occurs in patients who have significant scarring at the injection site,[3] which makes the tissue hard and less receptive to accepting the volume of fluid injected. Large amounts of simple edema fluid or lymphedema fluid at the injection site can result in erratic absorption of the medication and in medication loss since the injection tract cannot seal easily.
 Bleeding. Bleeding from the injection site is not uncommon. Significant bleeding and hematoma formation can occur if blood vessels are injured. This can be a difficult problem in patients who have bleeding tendencies or are taking antiplatelet medications or anticoagulants.[6] The person administering the IM injection should be adequately familiar with the anatomy of the region into which the medication is being given to avoid damage to blood vessels and subsequent bleeding complications. IM injections should be avoided in anticoagulated patients. Patients on antiplatelet agents should be watched closely following an IM injection to identify any bleeding problem.[6]
Bleeding. Bleeding from the injection site is not uncommon. Significant bleeding and hematoma formation can occur if blood vessels are injured. This can be a difficult problem in patients who have bleeding tendencies or are taking antiplatelet medications or anticoagulants.[6] The person administering the IM injection should be adequately familiar with the anatomy of the region into which the medication is being given to avoid damage to blood vessels and subsequent bleeding complications. IM injections should be avoided in anticoagulated patients. Patients on antiplatelet agents should be watched closely following an IM injection to identify any bleeding problem.[6]
Intravascular injections. None of the medications given by the IM route are safe to be given intraarterially.[7] This is a significant problem seen in drug users who administer drugs into arteries instead of veins.[8] Accidental intraarterial injection of medication during IM injection procedures was first reported in 1927 as a complication of bismuth injections in adults.[9] The majority of the reported cases of inadvertent injection of medication into arteries during attempted IM injections occur in children receiving injections in the buttock region.[10] The arteries most frequently involved are the inferior and superior gluteal arteries. The pressure exerted during the injection process can result in the medication being forced as far as the internal iliac artery to be redistributed throughout the leg.[10] This results in a severe chemical injury to the vessels with vasospasm and thrombosis. Skin necrosis, neurological damage, and loss of limb can follow. Prompt recognition and vascular surgical consultation is imperative. Despite all therapy available, a good outcome is difficult to achieve. Having personally taken care of a child with this problem, this author can attest to the frustration of dealing with this complication. Unfortunately, aspirating the syringe prior to injection of the medication to see if there is blood return does not assure that this problem will not occur.
Nerve injury. Nerve injury is another serious complication of IM injections and occurs more frequently than originally thought. During a five-year period from 1958 to 1963, an average of one case of nerve injury after IM injection was reported every three weeks to a medical liability insurance company.[4] Any nerve in the vicinity of the chosen injection site is likely to be damaged. The radial nerve is likely to be injured with injections in the deltoid or upper arm areas. The sciatic nerve is commonly injured by gluteal injections, especially in children.[10] In the past, children with foot drops were thought to have had "missed" cases of polio when in fact they had suffered injuries to their sciatic nerves with IM injections given during infancy.[10] These injuries were reported as early as the 1940s.[11,12] Sciatic nerve injury following injection is commonly manifested by paresis in the sciatic distribution followed by a causalgia or burning pain in the extremity several hours or days later.[13] Damage to motor function can be more severe, and recovery may be less complete.[14,15] One group reported that the diagnosis of sciatic palsy was made an average of 3.8 months following the intragluteal injection.[16] Radial nerve injury at the shoulder may be manifested by paresthesias in the distribution of the radial nerve and wrist drop.[4] Recent information has shown there is no specific medication that is neurotoxic when injected close to a nerve, but all will result in complete transverse necrosis of the nerve with extention of the necrosis to the exit of the nerve from the spinal cord if injected directly into any nerve.[4]
Pain. Pain during an IM injection generally is to be expected. Persistent pain, however, at the injection site is not an expected event. One series reports that persistent pain may occur in 23 percent of the patients who have complications.[3] The prolonged pain is usually due to irritation or chemical neuritis of a nerve; however, local muscle spasm due to the presence of the irritating medication has been faulted.[13] Continued pain at an IM injection site must be investigated to ensure it is not a symptom of an underlying abscess or other local problem. Many times this requires an MRI scan of the area as illustrated by Case 1 of this article. It is of interest that neither needle size nor needle length influence the degree of pain experienced at the time of the injection or the incidence of post-injection persistent pain.[4,6]
Abscess formation. Abscess formation at the site of an IM injection was the first recorded complication of the procedure.[2] It was the most common complication of IM injections in one study, occurring in 31 percent of patients who developed complications.[3] Infectious abscesses following IM injections are caused by the inoculation of the site with bacteria from the needle, syringe, or the medication. The bacteria can be carried to the tissues because of poor site preparation. Inadequately sterilized equipment and medications also can be responsible for inoculation of the area. The majority of these complications present with red, hot masses surrounding the previous injection sites. Occasionally, an abscess will rupture, and the site will be draining pus and liquid fat.[4] Incision and drainage of the area will result in marked improvement in the discomfort and will allow for cultures to be obtained to direct antibiotic therapy. The majority of these cases are seen within a few days to a few weeks following the injection;[4] however, in some cases, an abscess clinically may not be apparent for years after the injection as illustrated by Case 3 of this article. A high index of suspicion must be maintained for uncommon infectious problems after an injection, especially in the immunocompromised patient. For example, there is a report of a leukemia patient with no history of infectious problems who developed a localized mucormycosis infection at the site of an IM corticosteroid injection.[17]
More commonly, the abscesses that are seen at IM injection sites are sterile abscesses. These are nodules of liquefied fat and muscle resulting from necrosis of the involved tissues. Their development has been blamed on a hypersensitivity to the injected medication,[18] but more detailed research has shown that the problem develops when a caustic medication is injected in an inappropriate location.[19] When the medication is injected into the subcutaneous tissues rather than the muscle, absorption is delayed, which allows for a greater tissue reaction to the medication.[19] This reaction is manifested by local tissue necrosis and liquefaction with a surrounding area of intense inflammation. Thus, a painful nodule filled with sterile, liquefied tissue remains at the site. Many times this problem is caused by not using a needle of sufficient length to reach the muscle.[19]
Necrosis. Necrosis of the surrounding tissue following IM installation of a medication was not thought to occur unless the patient was allergic to the medication.[1] It has been found that necrosis of the muscle will occur after any IM injection no matter what medication is injected.[4] The only variable is the size of the necrotic lesion and the severity of it. Forceful placement of a volume of fluid into a closed space will cause damage. In other words, the surrounding muscle and tissues in the immediate area of the needle tip are subjected to the pressure of the mass of fluid that has been instilled into the area, which causes pressure necrosis. The toxicity of the medication, the volume injected, and even the speed at which the injection is given also will influence the size of the necrotic lesion.[20]
Numerous medications have gained notoriety for causing complications at IM injection sites. The significance and magnitude of the damage can be predicted by measuring the serum creatine phosphokinase activity following the injection.[21,22] Cephalothin sodium and tetracycline hydrochloride were the most frequent offenders in one study,[4] but the long-acting injectable medications have recently become the prime offenders.[5] Despite these reports it has been stated that the incidence of complications after administration of any specific agent is generally related to a medication's popularity.[4]
Scar formation. The significance of the necrosis may be negligible when few injections are given, but if multiple injections are given, especially in the same area over a protracted period of time, the areas of necrosis may become quite large and result in large areas of fibrosis of the tissues. This may be manifested by hard nodules felt deep in the tissues and even sunken areas of scar tissue seen on the surface of the skin. Dystrophic calcification of the scar tissue can occur with time resulting in even more painful areas. This is shown in Case 3 of this article. Once this occurs, operative excision of the area is the only therapy.
The muscle fibrosis from IM injections is a significant problem for veterinarians as well. The fibrotic scar that occurs in cattle following IM injection of medications may result in meat that is not suitable for the consumer and makes the remainder of the meat tough.[23] The losses to the meat producers runs into the millions of dollars annually.[23] It is apparent that the damage from IM injections is not just suffered by man.
Contracture of joints. Numerous reports have shown that in humans fibrosis of the extremity muscles following IM injections can result in contracture of joints. The local damage caused by the injected medication plus the local pressure necrosis causes the muscles to scar and shorten.[24] This causes the extremity to be held in an abnormal position, prevents normal range of motion, and can dislocate an extremity. This problem has been reported in the shoulder due to deltoid fibrosis,[24-28] the hip due to gluteal fibrosis,[16,28] and the knee due to quadriceps fibrosis.[29-31] In a thorough review of the subject of muscle fibrosis, Brodersen concludes that the majority of the muscle fibrotic complications and contractures were not apparent until the advent and widespread use of IM injections.[27] Repeated IM injections causes damage to the muscle with development of the fibrosis.[27] Treatment of these problems requires operative release of the fibrotic contractures and intensive postoperative physical therapy.[24,27] Treatment with physical therapy, use of nonsteroidal agents, and stretching are not effective.[27] It is of interest that, according to Ogawa, et al. (as quoted by Brodersen) no new cases of deltoid contracture in Japan have been reported since the dangers of IM injection were pointed out in 1975.[27]
Malignancy. Despite the severity of the previously discussed problems, a far more disturbing complication has been reported following IM injections -- the development of malignancies at injection sites.[32,33] The reported tumors have all been forms of sarcoma. There has not been a common medication injected in patients who developed the malignancies. Even though the incidences must be extremely low, any patient who has had an IM injection and continues to complain of a painful nodule at the injection site well after the injection should be thoroughly examined.
Complications of IM injections
Seeping of injected solution
Bleeding from the injection site
Hematoma
Intravascular injection
Nerve injury
Pain
Abscess
Necrosis of tissue
Scar formation
Contracture of joints
Malignancy
Avoidance of IM injection site complications
Determine landmarks
Clean skin thoroughly before inserting needleUse disposable syringes
Use needle of adequate length
Use needle of adequate length
Inject medication only into muscle, not fat
Avoid injecting during needle insertion
Aspirate syringe prior to injectingAvoid repeated injections into the same site
_______
 What is an intramuscular (IM) injection?
What is an intramuscular (IM) injection?
A technique to deliver a medication into muscle tissue for it's eventual absorption into the systemic circulation. Steroids, both oil and water-based, are administered this way.
 What is a subcutaneous (sub-q) injection?
What is a subcutaneous (sub-q) injection?
A technique to deliver a medication into the soft tissue (fat) immediately underlying the skin. Insulin, HCG, and HGH are typically administered this way.
What is aspiration?
To aspirate is to withdraw fluid with a syringe. More specifically, after inserting the needle, pulling back on the plunger of the syringe for a few seconds to see if the needle is in a blood vessel. Rarely, this will be the case and a bit of blood will fill the syringe. If this happens the needle should be removed, replaced with a new one, and another injection site should be used. And yes, if there is a little blood in your syringe, it is ok to inject it along with your steroid once you have found a different spot..........it's your own blood isn't it?
When aspirating, nothing should come back into the syringe if you are in the right spot. Pulling back on the plunger will create a vacuum in your syringe. The oil cannot expand to fill that space, but any air bubbles in your syringe will. You may notice the tiny bubbles getting bigger and bigger as you pull back. They will return to normal size as you release the plunger. If the air bubbles do not disappear upon releasing the plunger, you have an air leak most likely caused by the needle not being screwed onto the syringe tightly enough, although on very rare occasions, the syringe or needle itself can be defective. Either way, purge the air bubbles out, put a new needle on and try it again.
Do I really need to aspirate?
Those who inject without aspirating are taking unnecessary chances. Sweating, nausea, dizziness, severe coughing, breathing difficulties, anaphylactic shock, coma or death can all result from not aspirating. Most of the time, steroid users experience dizziness and coughing fits when they inject into a blood vessel. But you need to be aware of the dangers of neglecting this simple technique that should take about 3-5 seconds of your time.
 What exactly is an abscess?
What exactly is an abscess?
Abscesses occur when an area of tissue becomes infected and the body is able to "wall off" the infection and keep it from spreading. White blood cells migrate through the walls of the blood vessels into the area of the infection and collect within the damaged tissue. During this process, pus forms (an accumulation of fluid, living and dead white blood cells, dead tissue, and bacteria or other foreign invaders or materials).
Abscesses can form in almost every part of the body and may be caused by bacteria, parasites, or foreign materials. Most of the time, it is caused by unsanitary injection techniques. On very rare occasions, it can be caused by foreign particles your gear (a greater chance of this occurs when using/making a homebrew). The abscesses that we are concerned about are usually reddish, raised, and painful.
How do they treat an abscess?
Antibiotics are often given to aid the cure of an abscess but the real cure is generally surgical. A doctor would open the thing up and allow the pus to drain, then the body would take care of the infection. Some have even gone so far as to "drain" their own abscesses by inserting a needle/syringe into the abscessed area and drawing out the accumulated pus, although this is not recommended.
Can I reuse the same needle?
Yes, but only if you are an idiot or cannot obtain anymore needles. There really is no need to explain why you shouldn't re-use a needle. Common sense should kick in here, but the bottom line of re-using needles is an INCREASED CHANCE OF INFECTION. If you have trouble obtaining needles in your area, try finding a different way of getting them. The hassle of finding a source is negligible compared to the hassle of the abscess in your ass that would most-likely require a doctor and a scalpel. There are methods to "sterilize" a needle for re-use, but I will not delve into them. If you are still considering re-using a needle, re-read the above two questions.
Can I inject with the same needle I draw with?
Yes, but it is preferable to switch the needle out with a new one. The needle dulls significantly when pushed into the rubber stopper of your vial or scraped along the bottom of your amp. You may not notice the difference if you inject into your glute, but try injecting into an area that has more nerve endings such as a delt or bicep and you will notice immediately.
Does it matter if I push the needle in fast or slow?
I would recommend slowly, but this is personal preference. A lot of people will tell you to jab the needle in quickly. These people usually stop that practice after the first time they hit a nerve going in at full speed (usually quad shots). By going in slowly, you'll have more time to react if you hit a nerve.
Where exactly do I inject?
A picture is worth a thousand words.
www.spotinjections.com
//juicedmuscle.com/jmblog/content/site-injections-progress-or-madness
//juicedmuscle.com/jmblog/content/site-injections-part-2
Location of injections
 Glute injection:
Glute injection:
The best way to locate the correct place for dosing is to find the upper outer quadrant (section) of the butt cheek you are injecting into. Inject only into the upper outer erea of the quadrant – which muscle you actually inject into is less significant. It is important to avoid the other quadrants because they can be very sensitive to needle injection and there is a chance to hit the large veins and /or nerves.
Thigh injections:
The injectionspot is generally located on the front outside erea of the thigh between one hand’s width above the knee and one hand’s width below the hip joint. The injection should go into the thick erea of the large muscle to be sure to stay away from any bone.
outside erea of the thigh between one hand’s width above the knee and one hand’s width below the hip joint. The injection should go into the thick erea of the large muscle to be sure to stay away from any bone.
 Deltoid injection:
Deltoid injection:
Insert the needle at a 90-degree angle, or slightly angled up, into the middle of the deltoid muscle. This is approximately 2-4 finger-widths below the bony end of your shoulder bone and forms a triangle when you look at it from the side.
On YouTube are many clips showing the diverse injection techniques
 What gauge needles should I use?
What gauge needles should I use?
for drawing - 20g, 21g
18g needles are too big and they will eat up your stoppers in a hurry. A bigger hole means an increased chance of letting some little nasties into your sterile vial. Sometimes, the 18g will take out little chunks of rubber that fall nicely into your vial. That is not something you want. Imagine injecting that tiny piece of rubber into your muscle. I'll bet the doctor would have lots of fun digging into your muscle trying to find it and mutilating your muscle in the process.....
for injecting - 22g, 23g, 25g - for oil-based steroids, 27g, 29g - for insulin, HCG, HGH, and some water-based steroids. 21g-25g for some lower quality types of winny or suspension, higher quality versions can use a smaller needle generally.
22g and 23g are fine for glutes and quads. 25g is preferred for the smaller muscles such as delts, biceps, triceps, etc.
The smaller the gauge, the thicker the needle. An 18g is much thicker than a 22g.
What length needles should I use?
Most people can get by with a 1" needle, but if you have a higher percentage of body fat or are just plain big you should use a 1.5" needle to insure that you get deep into the muscle. You should only use a 1.5" needle for glutes, or if you have huge quads. For smaller muscle groups, 1" is the most common, although some people like to use a 5/8".
How many ccs can I shoot in one place?
It depends on how big you are. A general guideline is 1cc for delts, 2cc for quads, and up to 3ccs for glutes. Some do more, some do less......it all depends. After a cycle or two, you will know what your body can handle. If you are injecting into other muscles such as biceps, triceps, or calves, it's best to start off with a small volume and work your way up.
Can I pre-load my syringes?
If at all possible, leave it in the vial or amp. If you need to pre-load, just keep in mind that the syringe must be stored safely. Nothing sucks more than having the plunger pushed in accidentally and losing some of your gear.
Which is the best brand of needle?
Terumo, B-D, and Monoject are the primary manufacturers of needles/syringes. Both Terumo and B-D have an ultra-thin wall design (the wall of the needle is thinner, so more fluid can pass through the same gauge of needle). From personal experience as well as opinions from many other steroid users, Terumo seems to be the sharpest.
Common "FREAK OUTS"
I can't get all the tiny air bubbles out of my syringe....
As long as you tap it and get most of the air out, you will be fine. A little air intramuscular won't hurt you. According to the USH2 by Dan Ducaine, it supposedly takes about 10ccs of air injected into a blood vessel to kill you. I wonder how the hell they figured that one out.
I saw blood in the syringe after I pulled out....
You passed through a blood vessel and a little bit of blood entered the syringe on the way out. No biggie.
I pulled the needle out and blood dripped/squirted out....
You passed through a blood vessel. Apply a little pressure with your alcohol swab. You'll live.
I pulled the needle out and oil was dribbling out....
You injected too much in one place or you didn't inject deep enough. No biggie. Try injecting slower or leaving the needle in you for 30 seconds after you have injected it all. This should give the oil some time to dissipate so very little, if any, should dribble out.
I injected into my quad, and my leg was twitching....
You grazed a nerve. Usually it's a good idea to pull out and try another spot.
I don't think I injected deep enough....
If you think you injected into a layer of fat, don't worry. It will just take longer for the steroid to dissipate than it would if you had injected into the muscle. Eventually it will be absorbed. Don't let anyone tell you that you wasted it because that is not true.
I want to mix two different steroids and combine them into one syringe. How do I do this?
Let's say you want 1cc of deca and 1cc of test. First, draw 1cc of air and inject into your vial of deca. Withdraw 1cc of deca and pull the needle out. With the needle pointing up, draw 1cc of air into your syringe (your plunger will be at the 2cc mark - 1cc of deca in it and 1cc of air you just drew into it). With the needle pointing up, inject that 1cc of air into your vial of test. Withdraw 1cc of test. You now have 1cc of deca and 1cc of test in the same syringe. Don't forget to change the needle before you inject.
Instructions for first-timers.....
Step 1
Wash your hands.
Step 2
Wipe the top of the vial of medication for injection with an alcohol swab.
Remove the needle guard from the needle and syringe, saving the needle guard. Be sure you are using a proper syringe for intramuscular injections. Pull back on the syringe plunger to draw up an amount of air equal to the amount of oil you want to inject (pic). For example, if you want to inject 2ccs of oil, then pull back 2ccs of air.
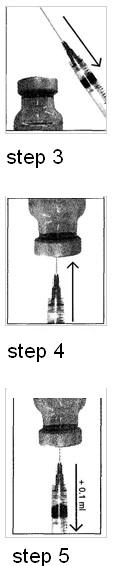
Step 4
Holding the vial of medication in an upright position, insert the needle straight through the center of the rubber stopper in the vial. Then push the plunger to discharge all the air into the vial.
Step 5
With the needle in the vial, turn the vial upside down and hold it in one hand. The tip of the needle should be in the solution. Using your free hand, pull the plunger back in a slow, continuous motion until you have drawn into the syringe the amount of medication that your doctor has prescribed.
Step 6
If air bubbles have formed in the syringe, dislodge them by gently tapping the syringe with your free hand while continuing to hold the syringe and vial in the inverted position. Bubbles should rise to the top of the syringe, and then you can push them back into the vial by moving the plunger. Double check to make sure you have the correct amount of medication in the syringe. If necessary, draw more solution into the syringe.
Step 7
Remove the needle from the vial. With the needle pointing upwards, pull back on the plunger until all oil from the needle has been pulled back into the syringe. Unscrew needle from syringe and replace with a brand new, preferrably smaller needle. Replace needle guard.
Step 8
Prepare the injection site by cleaning the area with an alcohol swab. To do this start at the center, apply pressure, and cleanse in a circular motion working outward. Do not retrace your steps.
Step 9
Wait a few seconds until the alcohol has dried. This reduces the sting. Remove the needle guard from the needle and syringe. With the needle pointing upwards, tap the syringe to dislodge the air bubbles and push the air out of the needle until you see a tiny drop of oil start to form at the tip. Hold the syringe as you would a pencil.
Step 10
Holding the syringe at a right angle (perpendicular) to the prepared injection site and insert the needle.
Step 11
When the needle is in place, slowly pull back on the plunger to see if any blood flows into the syringe. If some blood does enter the syringe (a rare occurrence), remove the needle, replace the needle with a new one, find another area to inject. Repeat Step 8.
Step 12
If no blood enters the syringe, slowly inject the medication by gently pushing the plunger until the syringe is empty.
Step 13
Remove the needle quickly. Apply pressure to the injection site with your alcohol swab. You're done. Massage the area. Now go do the most important parts
Use some ice and that really helpes inflammation. Slight fever, but achey. Doxycycline helps with that.
- Login to post comments


