site injections part 2
I want it all – and – I want it now
.jpg) As you could read in part 1 of this article, the bodybuilding culture is changing and it is changing fast. People want instant solution, instant results.
As you could read in part 1 of this article, the bodybuilding culture is changing and it is changing fast. People want instant solution, instant results.
This raises concern among people that want to inform and warn, these mostly young and naïve newbies. There are many websites, forums and booklets that inform potential users that are interested in shortcuts to increase their muscle mass. On these forums certain members manifests themselves as experienced people, most of the time these guys, or groups of guys, sell the homebrews and or veterinary compounds ( Kynoselen – ADE - Potenay) they are hyping.
We all know bodybuilding is a sport that takes a long time and demands a lot of time, determination and dedication. The use of anabolic androgenic steroids was the first shortcut. That decreased the time necessary to achieve that desired muscular physique. Then came the insulin and peptides. After the professionals showed us the way now also cosmetic bodybuilders are starting to use implants and injectable implants. We want to inform about the (possible) consequences of all these new procedures, to balance the misconceptions and even the deliberate misinformation provided by many websites that want or need to please their sponsors. Reading some of these threads on bodybuilding boards really worries me. Low risks and easy gained muscles are promised.
There is a ( severe) risk that, mostly young people, who live train in environments where identity, confidence and respect are increased proportionately with muscle volume. And the use of AAS and site injection oils to provide muscle growth is legitimate and broadly accepted. But even a brief experimental period can cause permanent, destructive complications.
An intramuscular injection is an invasive procedure. Site injection deep under the muscle belly, to produce an increase in muscle mass and a “lifting effect”, is even more invasive. Its extremely important to do this as sterile as possible, in fact you or your assistant are performing a cosmetical operation. Such a surgery should be performed in a sterile room, with sterile clothes and washing with a sterilising agent etc etc, I bet you’ve seen an cosmetic operation on the TV.
 An other important issue is that most users opt to buy a cheap products, mostly bought from people that manufacture their own mixes of site injection oils mixed with steroids, either water based or oil based, short esters and no esters (base). They still want to make profit and mostly use vegetable or mineral oils, and then mostly the ones from grocery store, the heat it the stove, filter it and then it should be fine. A pharmaceutical oil is to expensive ..and don’t be mistaken, the same goes for injectable anabolic steroid compounds. Who cares for plant collagen etc. You won’t notice the destructive consequences, at least mostly not directly.
An other important issue is that most users opt to buy a cheap products, mostly bought from people that manufacture their own mixes of site injection oils mixed with steroids, either water based or oil based, short esters and no esters (base). They still want to make profit and mostly use vegetable or mineral oils, and then mostly the ones from grocery store, the heat it the stove, filter it and then it should be fine. A pharmaceutical oil is to expensive ..and don’t be mistaken, the same goes for injectable anabolic steroid compounds. Who cares for plant collagen etc. You won’t notice the destructive consequences, at least mostly not directly.
Don’t wanna scare you, but want to show some case reports, even though the media showed the devastating effects of silicones used to firm and increase female breasts.Injection of paraffin oil to change physical configuration is an obsolete procedure from 1899, revived by bodybuilders as an alternative to intramuscular injections of steroids and or Site injection oils.
Injection of foreign substances, such as paraffin oil, for the purpose of body contour augmentation has been used from the beginning of the last century . Since the severe destructive consequences of migrating paraffin oil were recognized, the procedure has become obsolete in Western medicine. However, oil injections are still practised, either as self-injection or by unauthorised personnel. Adverse effects include skin inflammation, indurations, sterile abscesses, fistulas, and skin rupture with suppuration of oily material.
Among bodybuilders, many cases have been reported in which all had performed oil injection for the purpose of muscle augmentation. We
describe here another case from this subculture in which the person developed skin and muscle necroses forming multiple ulcers after paraffin oil injections. The ulcers healed after conservative treatment with compression bandage. However, this patient may suffer from long-term sequelae, such as the formation of paraffinomas, which may require further surgical treatment
 A 23-year-old male bodybuilder was referred to Copenhagen Wound Care Centre with numerous ulcers on both upper arms (Fig. A). Previously, he had presented to different regional hospitals. For the purpose of muscle augmentation, he had injected paraffin oil in the biceps, triceps and anterior/posterior part of the deltoid muscle. Over a period of 1–1.5 years, he carried out 10 series of oil injections of 20 ml in each muscle. In total, he had injected approximately 1 litre of oil in each arm. At the same time he also abused anabolic steroids. Approximately one month after the last series of oil injections, he developed increasing pain in both arms.
A 23-year-old male bodybuilder was referred to Copenhagen Wound Care Centre with numerous ulcers on both upper arms (Fig. A). Previously, he had presented to different regional hospitals. For the purpose of muscle augmentation, he had injected paraffin oil in the biceps, triceps and anterior/posterior part of the deltoid muscle. Over a period of 1–1.5 years, he carried out 10 series of oil injections of 20 ml in each muscle. In total, he had injected approximately 1 litre of oil in each arm. At the same time he also abused anabolic steroids. Approximately one month after the last series of oil injections, he developed increasing pain in both arms.
He also complained of malaise and temperature. The skin covering the deltoid region and the brachial anterior region was red, swollen and indurated. Enlarged painless lymphatic nodes were found in the neck, but none in the axillae. Laboratory examinations showed increased infection parameters. Ultrasound showed multiple echo-empty structures of different sizes compatible with oil but no abscesses. At this time no treatment was given.
 Over the next 2 months, skin necroses developed with spontaneous perforation and suppuration of oily, necrotic material leaving numerous ulcers in both arms. The largest one was approximately 7-15 cm. A larger abscess-like structure over the right pectoral muscle was punctured twice with extraction of blood blended with oil. Microbiological culture of the material showed no pathogens (A).
Over the next 2 months, skin necroses developed with spontaneous perforation and suppuration of oily, necrotic material leaving numerous ulcers in both arms. The largest one was approximately 7-15 cm. A larger abscess-like structure over the right pectoral muscle was punctured twice with extraction of blood blended with oil. Microbiological culture of the material showed no pathogens (A).
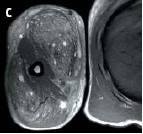
To evaluate the possibilities for surgery, magnetic resonance imaging (MRI) of both arms was performed (C). MRI gave an almost identical picture to that of ultrasound. The biceps muscles showed small cystic and confluent areas corresponding to the paraffin oil. Almost equivalent changes were seen in the triceps musculature. No abscesses or fistulas were seen. Because of the extensive spread of the oil, it was not possible to perform surgery.
At Copenhagen Wound Care Centre, he was treated with dicloxacillin and compression bandage from the wrists and up to the shoulder region. Against doctors advice, our friend did not show up for further management until 1.5 years later. During that time, he had used compression therapy on himself, for as long as possible and he observed improvement and even complete healing of the wounds with that treatment (B). However, he developed several sore firm tumours on both arms including smaller ones around the nipple area, probably representing paraffinomas. He was referred to plastic surgery.
The term paraffinoma describes the tumours caused by granulomatous reaction to paraffin (mineral oil) or other lipophilic (oily) substances introduced in the subcutis. Tumours are also sometimes designated according to the injected substance as oleomas or siliconomas when oil or silicon, respectively, is injected. In general it is advisable to perform excisional surgery to remove as much of the injected material or affected area as possible. In some cases, as in the one described here, conservative treatment may be the only option, because of very deep and widespread distribution of the oil.
Who cares?
In 2010, our then 26 years old friend was admitted again to a Danish hospital. During the clinical interview, he revealed that he had recently finished a cycle of anabolic steroids and EPO. Over the course of the next few hours, our friend developed signs of multi-organ dysfunction and respiration difficulty and he transferred to the ICU (intensive care) . Monometric monitoring (bloodpressure messuring with a manchet) on the patients upper arms proved difficult. Jeez, really ? Invasive blood pressure monitoring revealed a hypertensive crises. The conclusion was that the multi-organ dysfunction was possibly caused by multi-substance-induced hypercalcemia. To be continued?
 Again from Brazil, where else, a 28 years young, white girl injected her butt and thighs with aesthetic purpose, she did not know the amount of material injected appeared erythematous and edematous lesions on the buttocks. Two month later that developed ulceration and drainage of oily secretion. Há 6 meses, sucederam lesões semelhantes na coxa esquerda e lesão tumoral mal delimitada na coxa direita.Four months, followed similar lesions in the left thigh and ill-defined tumor in the right thigh.
Again from Brazil, where else, a 28 years young, white girl injected her butt and thighs with aesthetic purpose, she did not know the amount of material injected appeared erythematous and edematous lesions on the buttocks. Two month later that developed ulceration and drainage of oily secretion. Há 6 meses, sucederam lesões semelhantes na coxa esquerda e lesão tumoral mal delimitada na coxa direita.Four months, followed similar lesions in the left thigh and ill-defined tumor in the right thigh.
The latency between application of the substance and the development of symptoms was relatively short, considering that there are reports in the literature whose manifestations begin until 40 years after this practice.
She probably planned on strolling along the Copacabana beach, with her hard round buttocks in a thong, but she makes a nice picture in this article, am I right??
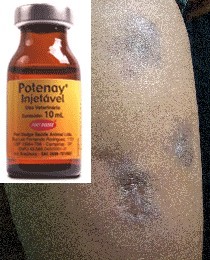 Again Brazil a case of ulcerated lesions secondary to infiltration oily material in a young man with purpose of increasing muscle mass and define the body contour. The treatment of these cases is quite complex, with unsatisfactory answers. No fever and systemic symptoms accompany the cutaneous manifestations. He reported ever having used steroids oral and injectable and an injectable multivitamin for animal use (Potenay ®) on other occasions. The use of tetracycline for a long period proved to be effective.
Again Brazil a case of ulcerated lesions secondary to infiltration oily material in a young man with purpose of increasing muscle mass and define the body contour. The treatment of these cases is quite complex, with unsatisfactory answers. No fever and systemic symptoms accompany the cutaneous manifestations. He reported ever having used steroids oral and injectable and an injectable multivitamin for animal use (Potenay ®) on other occasions. The use of tetracycline for a long period proved to be effective.
Bodybuilders tend to use means that are cheap and easily available in their homeland, and there are mostly hyped on forums there also. Something similar happened in France with Kynoselen and the results are comparable.
Potenay ® INJECTABLE is a composite of B vitamins and stimulants for veterinary use, the 10ml bottle costs about $ 7.00.Potenay is indicated "for the recovery of sick animals and that can never be understood as a substance or anabolic steroid, it is not recommended under any circumstances for human consumption." The consequences of applying the product to human health are unknown, since Potenay never been tested in humans, the company said. "There is no foundation in the use of our product and anabolic steroid like," says the director of the business of large animals from Fort Dodge.
 Methicillin-resistant Staphylococcus aureus abscess after intramuscular steroid injection
Methicillin-resistant Staphylococcus aureus abscess after intramuscular steroid injection
A 25-year-old bodybuilder was hospitalized with a painful left upper arm five days after injecting 1.5 ml of a steroid preparation into the medial aspect of his left biceps brachii muscle. He reported using a sterile needle obtained from a pharmacy, but the source of the steroid vial was unknown. At the injection site, there was a tender, erythematous, palpably fluctuant mass, 10 by 6 cm (Panels A and B). The level of creatine kinase was 18,100 U per liter, and the white-cell count was 20.6×103 per cubic millimeter. Computed tomography revealed a large abscess containing gas in the medial left upper arm (Panels C and D). The abscess was incised and drained, after which extensive débridement was performed. Microscopy of a skeletal-muscle sample showed acute necrotizing myositis, and culture of a swab from the deep wound revealed methicillin-resistant Staphylococcus aureus. Vancomycin was given intravenously, followed by oral trimethoprim–sulfamethoxazole. The wound healed well over the next several days. The patient was discharged home 15 days after the abscess had been drained. thickened subcutaneous retinaculae accented, probably reactive fibrotic changes
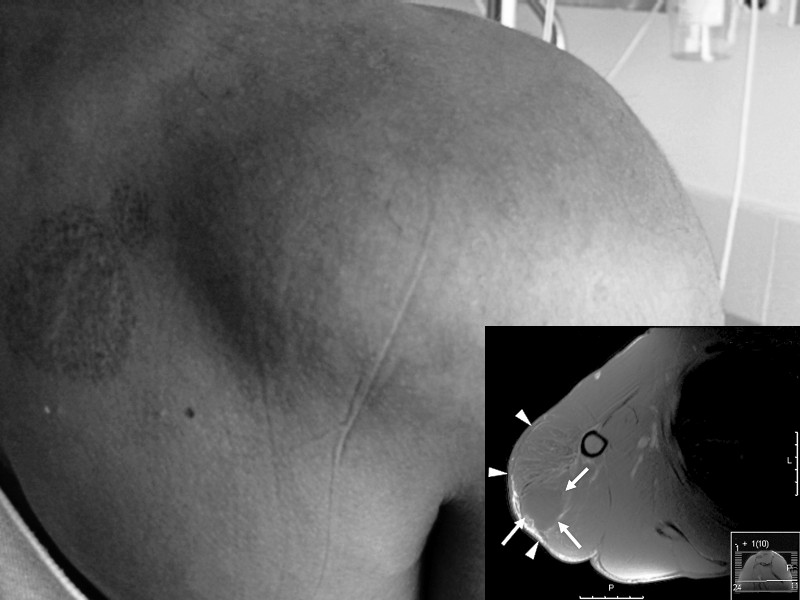 A 39-year-old amateur bodybuilder (picture) presented to the emergency department with excruciating pain and inability to move his right shoulder after injecting stanozolol, an anabolic-androgenic steroid (AAS), into his right deltoid muscle on the same day. On physical examination, the right deltoid muscle was swollen and tense and the surrounding skin red, tender, and warm. He had no fluctuation or systemic fever and no sensory or motor deficit. His distal pulsations were distinct. Laboratory test results suggested massive rhabdomyolysis (breakdown of skeletal muscle tissue). The major magnetic resonance imaging finding was diffuse hyperintensity signals on T2-weighted images of the deltoid muscle, which was consistent with edema. Doping" among amateur athletes occurs frequently. It can cause acute and chronic health problems, most of which are systemic. This is the first description of localized rhabdomyolysis in the area of an AAS injection.
A 39-year-old amateur bodybuilder (picture) presented to the emergency department with excruciating pain and inability to move his right shoulder after injecting stanozolol, an anabolic-androgenic steroid (AAS), into his right deltoid muscle on the same day. On physical examination, the right deltoid muscle was swollen and tense and the surrounding skin red, tender, and warm. He had no fluctuation or systemic fever and no sensory or motor deficit. His distal pulsations were distinct. Laboratory test results suggested massive rhabdomyolysis (breakdown of skeletal muscle tissue). The major magnetic resonance imaging finding was diffuse hyperintensity signals on T2-weighted images of the deltoid muscle, which was consistent with edema. Doping" among amateur athletes occurs frequently. It can cause acute and chronic health problems, most of which are systemic. This is the first description of localized rhabdomyolysis in the area of an AAS injection.
A 34-year-old Dutch bodybuilder presented at the emergency room with fever, vomiting and muscle cramps that had started during a bodybuilding session. Several days before he started training he had used tablets and intramuscular injections containing the anabolic steroids: dehydro-chloro-methyltestosterone, boldenone and trenbolone. In addition, he had taken clenbuterol tablets, liothyronine tablets and subcutaneous injections of phosphatidylcholine. Laboratory investigations revealed massive rhabdomyolysis *. The patient was treated with intravenous fluid replacement and sodium bicarbonate to alkalinize the urine. He recovered quickly and his renal function remained unaffected. 'Doping' among amateur athletes in the Netherlands occurs frequently. Apart from long term side-effects, doping can also cause acute health problems. Therefore it is important to ask about doping use during history taking in amateur athletes.
* Rhabdomyolysis is a condition in which damaged skeletal muscle tissue breaks down rapidly. This damage may be caused by physical (e.g. crush injury), chemical, or biological factors. Breakdown products of damaged muscle cells are released into the bloodstream; some of these, such as the protein myoglobin, are harmful to the kidney and may lead to kidney dysfunction. The severity of the symptoms (which may include muscle pains, vomiting and confusion) depends on the extent of the muscle damage, and whether kidney failure develops
 The British medical boards wrote down a similar story A 44-year-old bodybuilder HAPI also complained of pain, but he was no longer a beginner, it is the upper arm and chest pain, which was not a surprise after he spent 120 ml sesame oil per week. The picture can be seen that his right arm is swollen and red, also the right breast was deformed ( see picture).
The British medical boards wrote down a similar story A 44-year-old bodybuilder HAPI also complained of pain, but he was no longer a beginner, it is the upper arm and chest pain, which was not a surprise after he spent 120 ml sesame oil per week. The picture can be seen that his right arm is swollen and red, also the right breast was deformed ( see picture).
**This case report describes a 26-year-old body builder who had practiced several months of intramuscular self-injection of walnut oil. Apparently this is a normal procedure amongst body-builders. Our patient complained of swelling and tenderness overlying an injection site. Injections of oil may cause foreign body reactions, leading to tumours named according to the injected material; e.g. paraffinoma, oleoma. Systemic distribution has been reported to result in pulmonary complications.
 A 21-yr-old bodybuilder was admitted to our hospital with a severe case of myalgia and purpura. Onset was 1 week after intramuscular self-injections of 10 ml sesame oil in both biceps. He had used sesame oil on five previous occasions. On physical examination approximately 10 blue, itchy lesions with a maximum size of 36 cm2 on the shoulders, arms and legs were discovered
A 21-yr-old bodybuilder was admitted to our hospital with a severe case of myalgia and purpura. Onset was 1 week after intramuscular self-injections of 10 ml sesame oil in both biceps. He had used sesame oil on five previous occasions. On physical examination approximately 10 blue, itchy lesions with a maximum size of 36 cm2 on the shoulders, arms and legs were discovered
(Figure, lower panel) The lesions failed to blanch on applying pressure. Magnetic resonance imaging of the affected muscles showed extensive oedema, suggesting local necrosis. Pathological examination of a skin–muscle biopsy of affected skin revealed a severe panvasculitis with mixed inflammatory cell infiltrate, composed of predominantly eosinophils, some lymphocytes and neutrophils (Figure, upper panel). In this case it is very likely that the sesame oil injections caused an allergic reaction leading to vasculitis. The patient was treated with oral corticosteroids for 2 weeks and high-dose morphine injections in order to control his pain. After 4 weeks, recovery was complete.
Sesame oil is frequently used as a solvent. Moreover, it seems to be commonly used by bodybuilders [1]. In general, people should be more aware of possible allergic reactions to solvents like myalgia and vasculitis when using intramuscular drugs.
1.) Darsow U, Bruckbauer H, Worret W-I, Hofmann H, Ring J. Subcutaneous oleomas induced by self-injection of sesame seed oil for muscle augmentation. J Am Acad Dermatol 2000;42:292–4.
 In Marseille France a case of fat embolism following self injection of vegetable oil (sweet almond oil)in the penis. Although vegetable oil is a stable neutral fat under usual storage conditions, it caused fat embolism and pulmonary injury in this patient. We investigated this mechanism by compound analysis of the injected oil, transbronchial lung biopsy and special staining of alveolar macrophages. This is the first description of the human response to vegetable oil injection. These data should aid in the investigation of the side effects of many types of lipids which may be applied to humans for various purposes in the future.
In Marseille France a case of fat embolism following self injection of vegetable oil (sweet almond oil)in the penis. Although vegetable oil is a stable neutral fat under usual storage conditions, it caused fat embolism and pulmonary injury in this patient. We investigated this mechanism by compound analysis of the injected oil, transbronchial lung biopsy and special staining of alveolar macrophages. This is the first description of the human response to vegetable oil injection. These data should aid in the investigation of the side effects of many types of lipids which may be applied to humans for various purposes in the future.
A second case is a A 30-year-old heterosexual Bulgarian male, who self-inflicted, twice in a six-month-period, intra-urethral liquid paraffin and tied up his penis with a cord in order to achieve both enlargement and elongation. He arrived in our emergency department suffering from suprapubic pain; physical examination revealed a rather unique deformity of the penis. He finally refused any treatment and absconded.
Injections of mineral oils, like paraffin, have been used, more often in Eastern Europe and Asia, subcutaneously and according to our report, even intra-urethral, intending mainly to penile augmentation. Such materials can not be metabolized and a foreign-body-reaction occurs. As a result, health risks may need immediate intervention. This case also emphasizes on the inability of modern medicine to uncover established public misconceptions
Some cases of subcutaneous injected liquid substances like paraffin or vaseline into the urogenital region can be found in the literature mainly on purpose of penis circumference enlargement. This pathological entity is known as penile paraffinoma. In case no pathological finding is revealed, physical examination together with medical history, with emphasis on paraffin injections into urogenitalia, can presumably establish the diagnosis. It's not unusual that the formation of the granuloma appears even years after the injections. Eandi et al. in a case of a 71-year-old man reported that the development of the paraffinoma occurred forty years after a series of penile injections of unknown substances. Moon et al. contacted a survey on 357 imprisoned men who had injected mineral oils into the urogenital region with the use of a semi-structured questionnaire combined with psychological evaluation. At the majority of the respondents (78%) non-medical personnel has performed this procedure and their main motive was the fear of inferiority of their penis or the weak erectile function. Following the injection two thirds found no relief, nearly everyone (91%) was not satisfied with his penis afterwards and finally more than two-thirds wanted to remove the injected material. More recently, Pehlivanov et al. in a twenty-five-patient cohort study reported that the motivation of the majority of them was to enlarge penis's size and secondly to increase their sex partners' intercourse satisfaction. This study also emphasizes on the fact that non-medical personnel (60%) or the patients themselves (40%) did the injections.
 On this picture a Brazilian male that got an infection after injecting a site enhancement oil, was hospitalised and died later in the same hospital.
On this picture a Brazilian male that got an infection after injecting a site enhancement oil, was hospitalised and died later in the same hospital.
The following is quoting Cy Wilson from Testosterone magazine, over 5 years ago.
This crap is in no way permanent. Synthol is composed of geranium and lemon oils, menthol, resorcinol (a mild irritant), chloral hydrate (a hypnotic and sedative similar to barbiturates, with some small analgesic ability), as well as salicylic acid, which is used to treat corns by causing the tissue to swell, soften, then degrade and wear away. The resorcinol and salicylic acid are both dermatological compounds used to treat skin problems. They're meant to be applied topically. Not one of these compounds was meant for injection. I shudder just thinking about someone injecting this concoction into their arms.
The reason why it's not permanent is simply because the aforementioned ingredients cause nothing but swelling and inflammation due to irritation. As soon as the irritation is gone, the inflammation and muscle size increase is gone as well, leaving only the scar tissue. Even worse, if the muscle tissue reacts the same way that corns do to the salicylic acid, you end up with a loss of muscle tissue after the swelling subsides. So, if these guys aren't careful, they won't have to wait for old age to cause muscle tissue loss, because Synthol will take care of that for them.
Although I can't say there's concrete evidence that injecting salicylic acid into muscle will produce these results, I sure wouldn't take the chance. Along the same lines is the fact that resorcinol, in high concentrations, may also interfere with thyroid production. The real kicker is that these are the risks involved if you are lucky enough to get the legitimate version. Otherwise, only God, and possibly a dealer somewhere, knows what's in that bottle. It's best to stay away from Synthol and its copycats
The list of severe complications is sheer endless, but I think you got the picture. The administration of all advertised means is not as harmless as many people want you to be believe. On the other hand if you educate yourself and buy with knowledge and common sense, you should be fine. Like we heard from a welknown T.V seri “Lets be carefull out there”.
The movieclip from the Brazilian synthol user, for those with a strong stomach
- Login to post comments


