A famous professor gives his refreshing opinion on GH in bodybuilding
 What once happened with the use of anabolic steroids now happens with growth hormone. Let me explain. When steroids where developed many scientists and pharmaceutical companies where convinced that modifications on the parent hormones would lead to favorable medication. In the golden era of steroid synthesis the main goal was to synthesize a compound which retained a high degree of anabolic activity coupled with a vastly diminished androgenic activity. In those days anabolic steroids where meant to be given to patients, to the old, the weak, the recovering, the undernourished etc. It was thought that through all these modifications one could create steroids that would serve many different purposes. Quite like nowadays many people think about recombinant human Growth Hormone. What followed was a pure demonization of anabolic steroids, the pharmaceutical companies unable to reach their goals exaggerated the side-effects just as other governmental institutions ..and the official media followed blindly. The bodybuilding community mistrusted the official medical research and was light-years ahead of official research. Some studies made such foolish assumptions that it made Will Brink in 1996 to write his classic article “walking the walk, or talking the talk” An article that said what most of us thought.
What once happened with the use of anabolic steroids now happens with growth hormone. Let me explain. When steroids where developed many scientists and pharmaceutical companies where convinced that modifications on the parent hormones would lead to favorable medication. In the golden era of steroid synthesis the main goal was to synthesize a compound which retained a high degree of anabolic activity coupled with a vastly diminished androgenic activity. In those days anabolic steroids where meant to be given to patients, to the old, the weak, the recovering, the undernourished etc. It was thought that through all these modifications one could create steroids that would serve many different purposes. Quite like nowadays many people think about recombinant human Growth Hormone. What followed was a pure demonization of anabolic steroids, the pharmaceutical companies unable to reach their goals exaggerated the side-effects just as other governmental institutions ..and the official media followed blindly. The bodybuilding community mistrusted the official medical research and was light-years ahead of official research. Some studies made such foolish assumptions that it made Will Brink in 1996 to write his classic article “walking the walk, or talking the talk” An article that said what most of us thought.
From this article , the researchers state: “Athletes often take androgenic steroids in an attempt to increase their strength. The efficacy of these substances for this purpose is unsubstantiated, (emphasis mine) however.” Unsubstantiated? Are they for real? Here is another statement from the study. “…but whether supra-physiological doses of testosterone or other anabolic-androgenic steroids augment muscle mass and strength in normal men is unknown.” Unknown? Unknown? Unknown to who? The next time you sit in the front row of a bodybuilding show or see some 280 pound androgen freak squatting the equivalent of a small family sedan, feel free to yell “hey fella(s), did you know that all those steroids you are taking have not been proven to build muscle!” LMAO !!!
In 1990, Dr. Daniel Rudman accomplished something that had never been done before. He reversed human aging. Wrinkles disappeared. Grey hair began turning black again. Energy levels soared. And seventy-year-olds had resurgence in sexual appetite.
 Twelve men, ages 61 to 81 volunteered for the trial. They received injections of a certain pituitary protein for 6 months. Usually, as we age, our skin grows thinner, we lose muscle and bone, and gain body fat. But the men in the study grew thicker skin, developed bigger muscles and denser bones and lost fat. On average, the participants experienced: 14.4% decrease in fat tissue mass, 8.8 % rise in lean body mass, 7.1% increase in skin thickness and a 1.6% rise in bone density. When Rudman’s study was published in the New England Journal of Medicine, he wrote: “The effects of six months of human growth hormone on lean body mass and adipose-tissue mass were equivalent in magnitude to the changes incurred during 10 to 20 years of aging.”
Twelve men, ages 61 to 81 volunteered for the trial. They received injections of a certain pituitary protein for 6 months. Usually, as we age, our skin grows thinner, we lose muscle and bone, and gain body fat. But the men in the study grew thicker skin, developed bigger muscles and denser bones and lost fat. On average, the participants experienced: 14.4% decrease in fat tissue mass, 8.8 % rise in lean body mass, 7.1% increase in skin thickness and a 1.6% rise in bone density. When Rudman’s study was published in the New England Journal of Medicine, he wrote: “The effects of six months of human growth hormone on lean body mass and adipose-tissue mass were equivalent in magnitude to the changes incurred during 10 to 20 years of aging.”
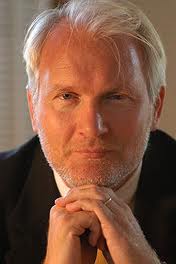
 Peter Sonksen
Peter Sonksen
In 2013 Melmed et all wrote: ”because fellow practitioners are over diagnosing the condition in order to legitimize undesirable practice.” This caused Peter Sonksen, an Emeritus Professor of Endocrinology, who had devoted most of his career on research towards insulin, GH and IGF, to write a refreshing editorial “Idiopathic Growth Hormone Deficiency in Adults, Ben Johnson and the Somatopause”. He gave credit to Daniel Duchaine as being a pioneer:
“Let us put this in context: athletes and their coaches were the first to discover the powerful anabolic actions of GH in adults. GH was given a glowing write-up by the California “doping guru” Daniel Duchaine in “The Underground Steroid Handbook” ; in 1982, he wrote: “We find that GH is the most expensive, most fashionable, and least understood of the new athletic drugs. It has firmly established itself in power-lifting and within a few years will be a commonly used drug in all strength athletics.”
Thus, human GH was established as a drug of abuse in sport some 7 years before the results of the first 2 randomized controlled trials confirming its powerful anabolic actions in humans were published in the bona fide medical literature. “
“A year earlier (1988), the sprinter Ben Johnson won a gold medal at the Olympic Games in Seoul, only to lose it 3 days later when his urine test confirmed that he had been taking the anabolic steroid stanozol; he subsequently admitted under oath that at the time he was also taking GH.
 These performance-enhancing effects of GH have now been confirmed using randomized controlled trials—first in abstinent, previously steroid-dependent athletes by Graham et al and, together with sex steroids in young athletes, by Meinhardt et al, 29 years after Duchaine’s first publication. I use these anecdotes to illustrate that it is not always the scientists who make the discoveries; sometimes, like the athletes, it is the people who are most likely to benefit and who are always hungry for an effective new therapy. If they find such a substance, try it, and find that it works, then the word spreads and later we, as clinician scientists, come along and discover it “officially.” Athletic competition is so strong and the rewards are so great that new ways of improving performance are constantly being sought. The intelligent athletes and their coaches are constantly using the “trial of one” paradigm to test new training regimes, diets, supplements, and substances. Athletes know their best performance for a given event to avery high degree of accuracy. It is not difficult for them to test out a range of potential performance-enhancing substances or techniques. Careful observations by athlete and coach make this a very powerful paradigm for evaluating new methods that is much more sensitive (and a great deal quicker and cheaper) than a standard randomized, double-blind, placebo-controlled trial.”
These performance-enhancing effects of GH have now been confirmed using randomized controlled trials—first in abstinent, previously steroid-dependent athletes by Graham et al and, together with sex steroids in young athletes, by Meinhardt et al, 29 years after Duchaine’s first publication. I use these anecdotes to illustrate that it is not always the scientists who make the discoveries; sometimes, like the athletes, it is the people who are most likely to benefit and who are always hungry for an effective new therapy. If they find such a substance, try it, and find that it works, then the word spreads and later we, as clinician scientists, come along and discover it “officially.” Athletic competition is so strong and the rewards are so great that new ways of improving performance are constantly being sought. The intelligent athletes and their coaches are constantly using the “trial of one” paradigm to test new training regimes, diets, supplements, and substances. Athletes know their best performance for a given event to avery high degree of accuracy. It is not difficult for them to test out a range of potential performance-enhancing substances or techniques. Careful observations by athlete and coach make this a very powerful paradigm for evaluating new methods that is much more sensitive (and a great deal quicker and cheaper) than a standard randomized, double-blind, placebo-controlled trial.”
Since 1990, there has been a strong (under) ground movement for the use of GH as a so-called “anti-aging” medication, which has not had the support of the medical establishment, particularly in the United States, where in 1993 the use of GH (along with anabolic steroids) was restricted by law to only those indications approved by “. . . the Secretary of Health and Human Services ”. In the United States, GH is only allowed to be prescribed for Food and Drug Administration (FDA)-approved conditions. The so-called “off-label” (at the discretion of the prescribing doctor) use is no longer permitted and indeed became a crime, punishable by imprisonment and/or a fine. I am not aware of another democratic country in the world where such harsh penalties are used to discourage medical practitioners from prescribing a drug that they might feel is the appropriate and beneficial treatment for a given patient.
In the 23 years since Rudman’s 1990 publication (14), there has accumulated a great deal more evidence that confirms and extends his original hypothesis. This includes a number of early short-term studies confirming powerful anabolic actions of GH, but many of these encountered too many adverse events. We now know that older people are very sensitive to GH, and these early studies, by using too high of a dosage, engendered these side effects.
Tandem (stacking rhGH with testosterone T)
In the last 10 years, 4 randomized controlled trials lasting from 14 to 26 weeks have shown convincingly that healthy normal older people can achieve tangible benefits from treatment with rhGH and that the beneficial effects can be enhanced by co-administration of sex steroids. This has been achieved using lower doses of rhGH and with minimal containable side effects. These studies, in addition to showing the favorable effects of rhGH on body composition, also showed that rhGH improved strength, mobility, and maximum oxygen uptake, particularly when it was combined with a sex steroid. The additive effects of T and GH in men have been shown to be dose-dependent. We have recently published a detailed review of the individual and combined effects of GH and T in older men.
Meinhardt et all stated in their study: “ Limitations: Growth hormone dosage may have been lower than used covertly by competitive athletes. The athletic significance of the observed improvements in sprint capacity is unclear, and the study was too small to draw conclusions about safety. Conclusion: Growth hormone supplementation influenced body composition and increased sprint capacity when administered alone and in combination with testosterone.”
 Oddly enough slowly research comes to acknowledge what we already knew for years. Where bodybuilders and athletes showed science the way. Now that studies are made to “prove” the anabolic effect of GH and insulin, professional bodybuilders used insulin, GH, T3/T4 (thyroid hormones) and IGF-1 LR3 and know these compounds have a synergistic effect. Of course it will take years and probably mainstream science will never be able to perform a study to this phenomenon because no ethic commission will allow a longtime cycle with such high doses of all kinds of hormones (poly-pharmacy). In the mean time we saw “in vivo” that professional bodybuilders became huge mass monsters with potbellies because of organ growth. The rest of their body also fall victim to this chemical warfare between the pro’s. I earlier described here: In the competitions the winner determines the general “winning Physique “ it’s all up to jury and the public of course, if they don’t want to see it anymore as with female bodybuilding, the mindset will change. Now the most massive bodybuilder wins. After a bulky Arnold, Frank Zane ruled with an aesthetically pleasing shape. It comes and goes. Who can tell when such a bodybuilder will stand up again. Old School bodybuilders like Arnold, Frank Zane, Mike Menzer, Franco Columbo and Lou Ferringo exited and inspired many people and bodybuilding became very popular.
Oddly enough slowly research comes to acknowledge what we already knew for years. Where bodybuilders and athletes showed science the way. Now that studies are made to “prove” the anabolic effect of GH and insulin, professional bodybuilders used insulin, GH, T3/T4 (thyroid hormones) and IGF-1 LR3 and know these compounds have a synergistic effect. Of course it will take years and probably mainstream science will never be able to perform a study to this phenomenon because no ethic commission will allow a longtime cycle with such high doses of all kinds of hormones (poly-pharmacy). In the mean time we saw “in vivo” that professional bodybuilders became huge mass monsters with potbellies because of organ growth. The rest of their body also fall victim to this chemical warfare between the pro’s. I earlier described here: In the competitions the winner determines the general “winning Physique “ it’s all up to jury and the public of course, if they don’t want to see it anymore as with female bodybuilding, the mindset will change. Now the most massive bodybuilder wins. After a bulky Arnold, Frank Zane ruled with an aesthetically pleasing shape. It comes and goes. Who can tell when such a bodybuilder will stand up again. Old School bodybuilders like Arnold, Frank Zane, Mike Menzer, Franco Columbo and Lou Ferringo exited and inspired many people and bodybuilding became very popular.
Pauses in the aging body and mind

Some scientists approach includes the extension of the concept of menopause to include a variety of “pauses,” which affect both men and women throughout life. Among these is the “andropause,” which most people are already familiar with. Once controversial, it’s now widely recognized that, much like women undergoing the “change of life,” aging men also undergo significant changes in hormone levels. These changes may have wide-ranging effects on well-being. Steady declines in the male sex hormone, testosterone, are known to “alter mood, memory, ability to concentrate, and the overall sense of vigor and well-being that may interact with a host of other psychologic changes associated with aging.” Another example is the “adrenopause,” characterized by deficits in important hormones such as DHEA and pregnenolone.
 Less familiar, but no less plausible, is the novel concept of “electropause,” or the gradual slowing of brainwave activity. Other proposed “pauses” include the “psychopause,” which involves age-related changes in mood, personality, and anxiety levels, and the “somatopause,” addressed in the first part of this blogpost, which is related to declining levels of human growth hormone. Not coincidentally, assessment of growth hormone plays an integral role in both the early diagnosis and treatment of cognitive decline.
Less familiar, but no less plausible, is the novel concept of “electropause,” or the gradual slowing of brainwave activity. Other proposed “pauses” include the “psychopause,” which involves age-related changes in mood, personality, and anxiety levels, and the “somatopause,” addressed in the first part of this blogpost, which is related to declining levels of human growth hormone. Not coincidentally, assessment of growth hormone plays an integral role in both the early diagnosis and treatment of cognitive decline.
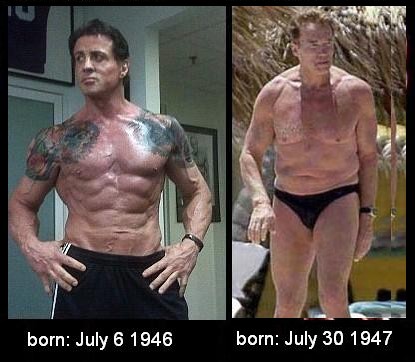
Both guys 62 years old, one on T and GH and maintaining to work-out. Don't get me wrong, I admire Arnold for his role in modern bodybuilding. But the picture makes painfully clear what bodybuilding is all about.
Scientific understanding regarding growth hormone and IGF-1—and their complex inter-relationships with the brain, the body, and aging—continues to evolve. One of the scientist in this field, Dr. Braverman is convinced that growth hormone holds one of the keys to restoring a degree of vitality and fostering repair in the aging body and mind. “I have seen astounding results with my patients’ use of growth hormone,” he writes, in a handout provided to his patients, “including vigor, physical strength, and more confidence in approaching life’s most difficult task: aging gracefully.” He believes that, combined with a bone density-enhancing drug, growth hormone represents the end of human frailty among thin, emaciated older people.
 As one team of scientists noted in a recent journal article: “[H]GH also affects metabolism, cardiac and immune function, mental agility, and aging.” Moreover, declining levels of growth hormone have been associated with decreasing lean muscle mass and increasing adipose tissue mass (body fat), along with thinning skin in aging individuals. In essence, at least part of the age-related tendency to lose strength and to gain girth may be attributed to declining growth hormone levels. Furthermore, growth hormone is intimately associated with a related hormone, insulin-like growth factor-1 (IGF-1), which, significantly, is capable of crossing the blood-brain barrier. Both are anabolic hormones. By definition, they stimulate the development of muscle mass, strength, and power. But their effects are more far-reaching than that. “Both GH and IGF-1 affect cognition and biochemistry in the adult brain,” wrote Swedish researchers recently. One of the mechanisms by which acetyl-L-carnitine helps protect against dementia is by boosting IGF-1 production. In an earlier paper, Dr. Sonntag and colleagues reported on experiments with growth hormone supplementation. “…Growth hormone administration to…humans raises plasma IGF-1 and results in increases in skeletal muscle and lean body mass, a decrease in [body fat], increased immune function, improvements in learning and memory, and increases in cardiovascular function.”
As one team of scientists noted in a recent journal article: “[H]GH also affects metabolism, cardiac and immune function, mental agility, and aging.” Moreover, declining levels of growth hormone have been associated with decreasing lean muscle mass and increasing adipose tissue mass (body fat), along with thinning skin in aging individuals. In essence, at least part of the age-related tendency to lose strength and to gain girth may be attributed to declining growth hormone levels. Furthermore, growth hormone is intimately associated with a related hormone, insulin-like growth factor-1 (IGF-1), which, significantly, is capable of crossing the blood-brain barrier. Both are anabolic hormones. By definition, they stimulate the development of muscle mass, strength, and power. But their effects are more far-reaching than that. “Both GH and IGF-1 affect cognition and biochemistry in the adult brain,” wrote Swedish researchers recently. One of the mechanisms by which acetyl-L-carnitine helps protect against dementia is by boosting IGF-1 production. In an earlier paper, Dr. Sonntag and colleagues reported on experiments with growth hormone supplementation. “…Growth hormone administration to…humans raises plasma IGF-1 and results in increases in skeletal muscle and lean body mass, a decrease in [body fat], increased immune function, improvements in learning and memory, and increases in cardiovascular function.”
Safety
Although there is still a need for more long-term safety data on rhGH administration to normal adults, we do have considerable long-term data on the safety of GH replacement in adults with GH deficiency from the post marketing surveillance and population-based studies. These have confirmed the overall safety of rhGH treatment and shown that there appears to be no evidence of serious adverse events or the development of cancer. On one hand, diagnosing GH deficiency in older people may be easy when the cause is immediately apparent (eg, pituitary tumor, surgery, etc). On the other hand, because it is well-recognized that GH secretion falls as we age and that by the time we’ve reached our late 60s and 70s our daily production of GH has fallen to levels overlapping from older people with pituitary tumors or post-surgery, many “normal” people in this older age group are therefore likely to be GH deficient. Thus, making a diagnosis of GH deficiency in older people may be more of a semantic issue than a medical issue. From a therapeutic point of view, not all of these people may benefit from or require treatment. The existing legal and financial rules on reimbursement in many countries limit the off-label use of GH, and because rhGH is still a very expensive drug, it makes it tempting for physicians to “shoehorn” the patient before them, whom they think might benefit from a trial of treatment with rhGH, into a diagnosis of idiopathic GH deficiency—the between-the lines message of Melmed’s update. Unlike Melmed, I believe that some of these patients will benefit from GH replacement. Of course, we would all want more long-term data on safety and efficacy of rhGH in older people, but those who are beginning to suffer the downward spiral of progressive weakness are looking for help now and cannot wait another 10 years for these results.
Of course In the USA many doctors earn a good living by prescribing GH and hormones in this is what Melmed meant.
Celibrities.
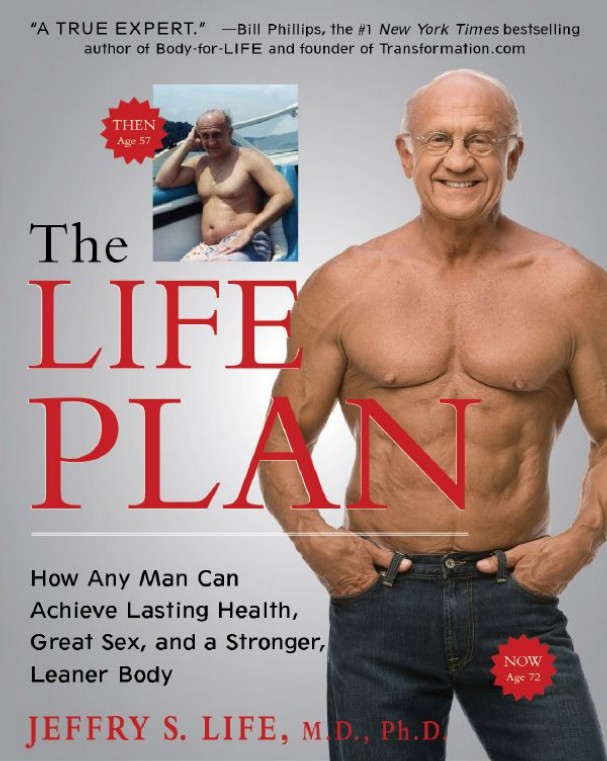
As described above the 1990 Rudman study caused a change in mindset. Many people wanted to preserve or restore their youthful looks and skills. Skeptics were politely handed copies of The New England Journal of Medicine.
This was exciting news to Big Pharma, whose favorite sons (Pfizer, Eli Lilly, Novo Nordisk) horned in on the action, sparking a marketing orgy that turned GH into a multi-billion-dollar industry.
One minute, GH was a godsend; the next, it was the scourge of the sports world. World-class athletes, in their never-ending quest to out-engineer one another, were “enhancing” themselves with whopping doses of GH often using it in tandem with anabolic steroids, testosterone, or other banned substances.
In the meantime, the Internet was flooded with a billion opportunists peddling half-baked H.G.H. creams, powders, and pills. Most of them didn’t have any effect but until now the scamproducts with so called GH flourishes. Overnight, it seemed, the country was filled with “longevity clinics” that prescribed GH to anyone with sniffles and a checkbook.
 And then came Suzanne Somers. In 2006, the onetime sitcom star published the magnum opus of her H.G.H. trilogy. That would be Ageless: The Naked Truth About Bioidentical Hormones. The book, which celebrated GH’s impact on the Seven Dwarfs of Menopause—Itchy, Bitchy, Sweaty, Sleepy, Bloated, Forgetful, and All-Dried-Up—was criticized by some doctors, including three who were quoted in the book. And it debuted at No. 1 on the New York Times best-seller list.
And then came Suzanne Somers. In 2006, the onetime sitcom star published the magnum opus of her H.G.H. trilogy. That would be Ageless: The Naked Truth About Bioidentical Hormones. The book, which celebrated GH’s impact on the Seven Dwarfs of Menopause—Itchy, Bitchy, Sweaty, Sleepy, Bloated, Forgetful, and All-Dried-Up—was criticized by some doctors, including three who were quoted in the book. And it debuted at No. 1 on the New York Times best-seller list.
The trend arrived in Hollywood by way of the city’s flourishing community of bodybuilders, who passed it on to their confederates in show business. Hollywood’s early adopters were action stars. The genre’s crown prince, Arnold Schwarzenegger, has denied ever using GH. But Sylvester Stallone and several other action stars are known to have taken it.
GH finally started entering the mainstream in the late 2000s. We know this because that’s when the MTV alerts started flying. In 2008 the Albany Times Union reported that Mary J. Blige, Timbaland, 50 Cent, Tyler Perry, and Wyclef Jean were among tens of thousands of people found to have received shipments of GH and steroids. None of the stars was accused of wrongdoing; the probe focused on doctors and pharmacies that illegally prescribed steroids.
But the biggest headline appeared around the same time: At Sydney Airport, in Australia—a country that tightly restricts GH.—a search of Stallone’s luggage revealed 48 vials of liquid youth. “H.G.H. is nothing,” the star later told People magazine. “Anyone who calls it a steroid is grossly misinformed Mark my words. In 10 years, it will be over-the-counter.”

Big Pharma cashes in on HGH abuse
In this Tuesday, June 28, 2011 photo, agents with the Drug Enforcement Administration stand outside the Treasure Coast Pharmacy in Jensen Beach after a raid. shortly before it opened Tuesday morning as part of an ongoing investigation. DEA, the Florida Department of Health, Florida State Troopers, Martin County Sheriff's deputies and Boca Raton and Margate police participated in the investigation.
The federal crackdown on illicit foreign supplies of human growth hormone has failed to stop rampant misuse, and instead has driven record sales of the drug by some of the world’s biggest pharmaceutical companies. The crackdown, which began in 2006, reduced the illegal flow of unregulated supplies from China, India and Mexico. But since then, Big Pharma has been satisfying the steady desires of U.S. users and abusers, including many who take the drug in the false hope of delaying aging.
An analysis of pharmaceutical company data shows that from 2005 to 2011, inflation-adjusted sales of HGH were up 69 percent. During the same period, sales of the average prescription drug rose 12 percent.
HGH: Court Rules in Favor of Pfizer on Off-Label Marketing Allegations
 On September 14 2010, the United States District Court for the District of Massachusetts issued a ruling that effectively ended a whistleblower’s attempts to bring attention to the off-label marketing of human growth hormone for anti-aging and other non-approved uses. Former Pfizer executive Dr. Peter Rost filed the qui tam claim in 2003. In short, Rost alleged that Pfizer improperly promoted its HGH drug Genotropin by providing kickbacks to physicians, including all-expense-paid trips to medical conferences in exotic locations.
On September 14 2010, the United States District Court for the District of Massachusetts issued a ruling that effectively ended a whistleblower’s attempts to bring attention to the off-label marketing of human growth hormone for anti-aging and other non-approved uses. Former Pfizer executive Dr. Peter Rost filed the qui tam claim in 2003. In short, Rost alleged that Pfizer improperly promoted its HGH drug Genotropin by providing kickbacks to physicians, including all-expense-paid trips to medical conferences in exotic locations.
Rost wasn’t exactly Mr. Popular at Pfizer. After he filed his qui tam, the company started dismantling his 60-person team, moving everybody but Rost from their New Jersey office to New York City. Then men in hardhats showed up and started knocking down the walls around him. Rost ultimately lost his job.
In 2005, the U.S. Dept. of Justice declined to join Rost in his suit and instead investigated Pfizer on its own. Two years later, in a settlement with the government, Pfizer paid a fine of $15 million and admitted that the unit that made Genotropin, Pharmacia, had promoted it for off-label uses such as anti-aging. (The company paid an additional $19.7 million fine related to a separate charge.) In an online posting, Rost dismissed the settlement as “equivalent to a speeding ticket”–a reference to the fact that Pfizer’s profit the previous year had been $11 billion.
Rost continued to fight his whistleblower claim, but it was a struggle. In 2008, a judge ruled that he could proceed as long as he focused only on allegations related to the promotion of HGH for the treatment of short children. His dream of exposing off-label use of HGH in anti-aging clinics was dead.
And now this latest ruling. It states that Rost failed to show that Pfizer’s promotion of HGH violated the False Claims Act. In other words, those activities did not result in improper claims being made to state Medicaid programs, as Rost alleged in his amended complaint. The ruling was made partially on the judge’s determination that the pharmacies that filled the prescriptions were “third parties” who were not knowledgeable about the marketing of the drug. If the pharmacy does not know that the prescription was written because a doctor was induced by the drugmaker to write it, she said, then there is no illegal false claim.
Jim Edwards, a blogger for BNET, concluded that this ruling “has made it easier for drug companies to bribe doctors with cash and gifts to prescribe their products.” I’m not sure I would go that far. But I will say this: Rost’s long and dramatic whistleblower story has come to a rather deflating end.


