Low Testosterone and Bloodwork
While low testosterone (“low T”) is more common among older men, it can also affect men under 30. What causes low T in young men?
Regardless of your age, a loss of sex drive, the development of impotence, and/or reduced muscle mass and strength; should give any knowledgeable doctor a red flag that T levels aren't on par.
Depression, fatigue, and loss of motivation are also commonly caused by low testosterone. Many of these symptoms can also be caused by other medical conditions or lifestyle factors. Unfortunately, many doctors would rather prescribe an antidepressant than bring back testosterone, a natural substance your body already makes, to a normal blood level.
L ow T is less common among young men, but it can still occur. Contributing factors include: high cholesterol levels, high blood pressure, being overweight or obese, drinking excessive amounts of alcohol, using illegal drugs, using anabolic steroids, taking certain prescription medications such as steroids and opiates, especially in excess. Living the good life in moderation, enjoying marihuana and wine doesn’t interfere with your Mr.O aspirations.
ow T is less common among young men, but it can still occur. Contributing factors include: high cholesterol levels, high blood pressure, being overweight or obese, drinking excessive amounts of alcohol, using illegal drugs, using anabolic steroids, taking certain prescription medications such as steroids and opiates, especially in excess. Living the good life in moderation, enjoying marihuana and wine doesn’t interfere with your Mr.O aspirations.
Men today have testosterone levels only one-third of those of our grandfathers living in their prime:
Y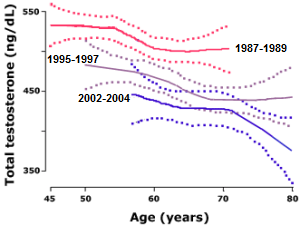 ounger and younger men are being treated more and more every day. It is not uncommon to see testosterone levels plateau and start declining in men around the age of 30. Some men are even being diagnosed as early as 25. One of the largest recent studies found strong evidence of a decline of more than 1.3% per year in men’s blood testosterone levels during the last two decades. We are facing an epidemic now with men having much lower testosterone levels then our fathers and grandfathers had. Low testosterone was almost non-existent before the 1980s.
ounger and younger men are being treated more and more every day. It is not uncommon to see testosterone levels plateau and start declining in men around the age of 30. Some men are even being diagnosed as early as 25. One of the largest recent studies found strong evidence of a decline of more than 1.3% per year in men’s blood testosterone levels during the last two decades. We are facing an epidemic now with men having much lower testosterone levels then our fathers and grandfathers had. Low testosterone was almost non-existent before the 1980s.
Part of the problem is the industrial revolution that began the advent of plastics, environmental toxins, estrogens, phthalates, and hormone-laden meats. The incessant onslaught of endocrine disruptors have been affecting our testosterone levels. Collectively, men have been becoming more effeminate by the year.
One example of an endocrine disruptor is Bisphenol A (BPA), commonly found in plastics. Bisphenol A enters our bodies when we eat our food stored in plastic containers or in BPA-lined cans. Microwaving food in plastic containers also releases more BPA into our food. When BPA enters our bodies, it is recognized as a type of estrogen and thus drives our testosterone levels down.
T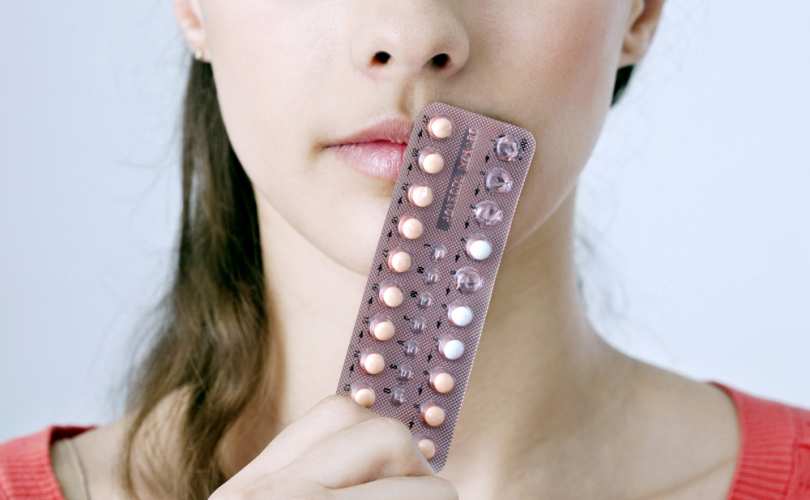 he hormone ethinyl-estradiol (EE2) is an active substance in many birth control pills which affects aquatic organisms when released as waste into the water. studies how fish are affected by EE2.
he hormone ethinyl-estradiol (EE2) is an active substance in many birth control pills which affects aquatic organisms when released as waste into the water. studies how fish are affected by EE2.
E ven low concentrations of EE2 have an impact on fish -- both their behaviour and their genetics. We have seen a change in the genetic balance in fish, and that they have a harder time catching food. Previous studies have shown that the fish also develop problems with procreation. This can lead to the complete disappearance of an entire fish population, and consequences for entire ecosystems Fish have more oestrogen receptors than humans, which makes them especially vulnerable to oestrogen in water. 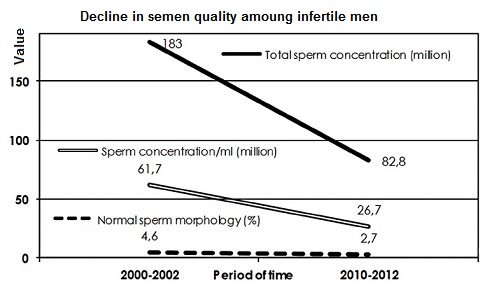 The thesis studies three different fish species: salmon, trout and roach, which are economically important fish that live in both sea and freshwater. Also, male reproductive organs are sensitive to estrogens, which interfere with normal function — estrogens have a contraceptive effect in males. EE2 has also been linked to testicular tumors.
The thesis studies three different fish species: salmon, trout and roach, which are economically important fish that live in both sea and freshwater. Also, male reproductive organs are sensitive to estrogens, which interfere with normal function — estrogens have a contraceptive effect in males. EE2 has also been linked to testicular tumors.
The barren left is so wedded to contracepted sex that they will brook no criticism of the means they use to ensure their sterility, even though, as the science shows, they sterilize other species in the process. Environmentalism meets the sexual revolution, and the sexual revolution wins.
A study conducted by the U.S. Geological Survey in 1999 and 2000 found measurable amounts of one or more medications in 80% of the water samples drawn from a network of 139 streams in 30 states. The drugs identified included a witches' brew of antibiotics, antidepressants, blood thinners, heart medications (ACE inhibitors, calcium-channel blockers, digoxin), hormones (estrogen, progesterone, testosterone), and painkillers. Scores of studies have been done since. Other drugs that have been found include caffeine (which, of course, comes from many other sources besides medications); carbamazepine, an antiseizure drug; fibrates, which improve cholesterol levels; and some fragrance chemicals (galaxolide and tonalide).
study conducted by the U.S. Geological Survey in 1999 and 2000 found measurable amounts of one or more medications in 80% of the water samples drawn from a network of 139 streams in 30 states. The drugs identified included a witches' brew of antibiotics, antidepressants, blood thinners, heart medications (ACE inhibitors, calcium-channel blockers, digoxin), hormones (estrogen, progesterone, testosterone), and painkillers. Scores of studies have been done since. Other drugs that have been found include caffeine (which, of course, comes from many other sources besides medications); carbamazepine, an antiseizure drug; fibrates, which improve cholesterol levels; and some fragrance chemicals (galaxolide and tonalide).
![]()
Depending on the lab your doctor uses, male testosterone levels typically range between 300ng/dl and 1000 ng/dl.
As you may well imagine, these ranges are not set to optimal levels. They are from a cross section of men aged 20 to 80; many of whom may be sick or diseased, from a lifetime of unhealthy habits.
If your blood w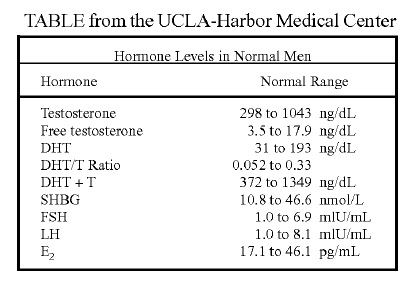 ork arrives, and your doctor happens to refuse treatment - even though your levels are close to the bottom of the range; then a gentle reminder of what optimal health entails may be in order.
ork arrives, and your doctor happens to refuse treatment - even though your levels are close to the bottom of the range; then a gentle reminder of what optimal health entails may be in order.
If you kindly point out, you have the T levels of a sick 80 year old (and feel like one at that); hopefully your doctor will come around.
Emphasize your Low Testosterone Symptoms
If your doctor is stubborn, or doesn't like their patients being active participants in their own healthcare - you may be better off emphasizing the symptoms more specific to low testosterone.
We recommend having your testosterone level as high as possible, 900-1000 (+/- ~100) ng/dl so long as you are under a physician's care, within acceptable ranges and are not experiencing any side effects.
What are free testosterone and bioavailable testosterone?
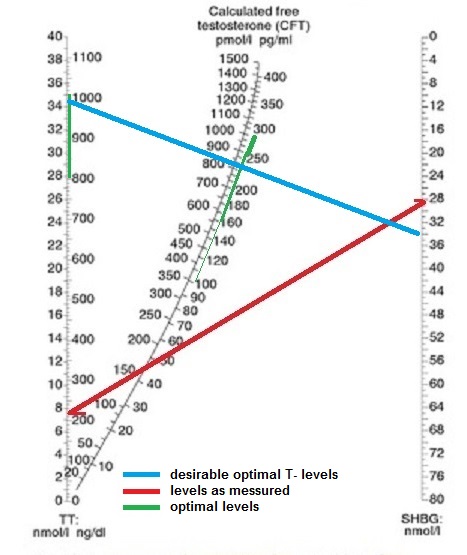
T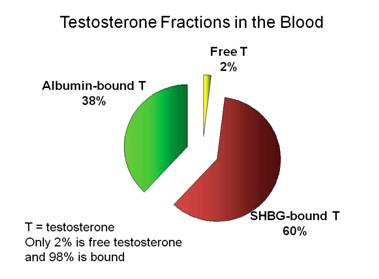 estosterone is present in the blood as "free" testosterone or bound testosterone (~98%). The latter may be loosely bound to albumin (about one-third), the main protein in the fluid portion of the blood, or bound to a specific binding protein called sex hormone binding globulin or SHBG (about two-thirds). The percentages in the three fractions varies greatly. The binding between testosterone and albumin is not very strong and is easily reversed, so the term bioavailable testosterone (BAT) refers to the sum of free testosterone plus albumin-bound testosterone.
estosterone is present in the blood as "free" testosterone or bound testosterone (~98%). The latter may be loosely bound to albumin (about one-third), the main protein in the fluid portion of the blood, or bound to a specific binding protein called sex hormone binding globulin or SHBG (about two-thirds). The percentages in the three fractions varies greatly. The binding between testosterone and albumin is not very strong and is easily reversed, so the term bioavailable testosterone (BAT) refers to the sum of free testosterone plus albumin-bound testosterone.
It is suggested that bioavailable testosterone represents the fraction of circulating testosterone that readily enters cells and better reflects the bioactivity of testosterone than does the simple measurement of serum total testosterone. Also, varying levels of SHBG can result in inaccurate measurements of bioavailable testosterone. Decreased SHBG levels can be seen in obesity, hypothyroidism, androgen use, and nephritic syndrome (a form of kidney disease). Increased levels are seen in cirrhosis, hyperthyroidism, and estrogen use. In these situations, measurement of free testosterone may be more useful.
For instance, the generally accepted normal range for a man’s total testosterone is 300-1000 ng/dl, and it’s considered normal to lose 1% of production per year after age 30.
N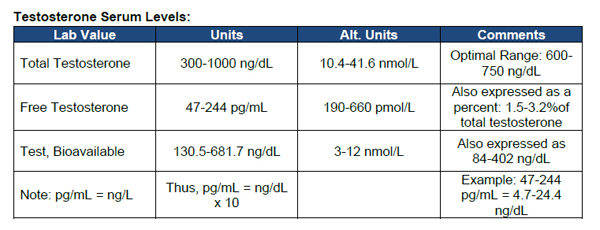 ow, since T levels should peak in your 20’s, let’s assume someone has a level of 750 ng/dl when they turn 30.
ow, since T levels should peak in your 20’s, let’s assume someone has a level of 750 ng/dl when they turn 30.
If you subtract 1% of production every year from a starting level of 750, you would have to live until you are 122 before your total testosterone levels would dip below 300 ng/dl.
The sales pitch for TRT reads like a wish list for every man on Earth: build muscle, trim fat, improve mood, recharge energy, crank up sex drive. No wonder prescriptions for the therapy have jumped 500 percent over the past 18 years. But while more men are trying TRT, a fierce debate rages among doctors about the safety and ethics of prescribing it to anyone without a defined deficiency.
Approximately 30 percent of men ages 40 to 79 are affected by hypogonadism, also called androgen deficiency, a condition marked by testosterone levels below 300 ng/dL (nanograms per deciliter), with symptoms that include muscle atrophy, weight gain, exhaustion, depression, bad sleep, disinterest in sex, and/or erectile dysfunction.
Before prescribing TRT for hypogonadism, a responsible doctor will recommend lifestyle changes to raise testosterone levels, including weight loss, exercise, and better sleep, says Dr. Harry Fisch, a professor of urology at Manhattan's Weill Cornell Medical College. Only when these modifications fail to cure a patient do TRT's benefits outweigh its risks, he adds.
The controversy surrounding TRT starts with doctors like Harvard Medical School's Dr. Abraham Morgentaler, who believes that more men suffer from hypogonadism than meet the condition's standards, he says that fading testosterone should be considered a treatable part of the aging process. "'Normal, healthy aging' is associated with bad eyes, bad hearing, bad teeth, bad joints, bad blood vessels, bad hearts, and cancer. We treat all of these to improve the quality of life or to increase longevity. Should we withhold offering prescription glasses to older men and women because poor vision is common with advancing years?"
O ther doctors take this argument even further, advocating that TRT should be used to make men as vigorous as possible, regardless of age. Dr. Jeffry Life, the buff 77-year-old star of many shirtless ads, became the poster boy for the Las Vegas–based Cenegenics Medical Institute precisely because his tremendous physique demonstrates how synthetic testosterone can help men defy expectations of frailty and physical decline. Dr. Elizabeth Yurth, says testosterone is "high-performance medicine" for people who don't want to grow old: "They want to be riding their bikes at 80." Her typical patient is a guy in his 40s or 50s who "can't keep up with his bike-riding buddies" – or with his wife in the bedroom. Testosterone can help change all that.
ther doctors take this argument even further, advocating that TRT should be used to make men as vigorous as possible, regardless of age. Dr. Jeffry Life, the buff 77-year-old star of many shirtless ads, became the poster boy for the Las Vegas–based Cenegenics Medical Institute precisely because his tremendous physique demonstrates how synthetic testosterone can help men defy expectations of frailty and physical decline. Dr. Elizabeth Yurth, says testosterone is "high-performance medicine" for people who don't want to grow old: "They want to be riding their bikes at 80." Her typical patient is a guy in his 40s or 50s who "can't keep up with his bike-riding buddies" – or with his wife in the bedroom. Testosterone can help change all that.
But it could also be argued that Yurth and Life are simply bringing men back up to the testosterone levels enjoyed by their forefathers. Population-wide, testosterone levels have dropped markedly in the past 20 years - 16 percent in 65- to 69-year-old men, for example. Obesity plays a role, since body fat helps turn testosterone into estrogen. But even when the research is corrected for weight and smoking, it suggests that other factors may be at play – environmental toxins, perhaps. A study from the University of California, for example, found that atrazine, a common pesticide, is so high in estrogen that it can transform an adult male frog into a fully reproducing female.
 Some doctors, like Life, believe that medicine's current standard of "low" – defined as anything under 300 ng/dL, with 500 to 700 considered healthy for men under age 40 – is too low and that men should aim for a higher optimal target. Life likes to boost patients' testosterone to 800 to 1,000 ng/dL, pointing to studies that show that men with testosterone levels in the upper 25 percent of normal have a lower risk of chronic disease.
Some doctors, like Life, believe that medicine's current standard of "low" – defined as anything under 300 ng/dL, with 500 to 700 considered healthy for men under age 40 – is too low and that men should aim for a higher optimal target. Life likes to boost patients' testosterone to 800 to 1,000 ng/dL, pointing to studies that show that men with testosterone levels in the upper 25 percent of normal have a lower risk of chronic disease.
"The typical story," Life explains, "is that you go first to a traditional MD and say, 'You know, I'm losing my edge. I'm going to the gym, but I dread it, and I'm losing muscle mass and strength, even though I'm working out, and I'm getting belly fat.' So they give you a blood test, and your hormone levels come back at 300. You're told you're normal, so you walk out thinking, 'I got normal testosterone. What's up?' What they won't tell you is that you're really a D student." And even if a doctor will treat you, Life adds, "he'll shoot for a new target of 350 to 400, making you a C student."

This bloodtest shows the tested guy has low T and low Free T and the levels of LH and FSH are on the low side of the reference range. On the nomogram you see the patients levels in red. If he wants to be in the optimal range he would want his testosterone levels between 800 and 1000 ng/dl (blue line) which when his SHGB level is optimal on 34 nmol/l would bring his free-T level close to the desirable range of 200 – 250 ng/dl. A cautious guy should not switch for optimal levels though, but gradual increase the dose to 500 to 700 ng/dl or even to average low levels. Don’t forget nobody is the same, and some guys feel perfectly well on these doses.
Others doctors warn that there could be a downside to having high testosterone, and that our bodies lower production for good reasons.
And the Northwestern study makes the point that lower testosterone levels in fathers may be an evolutionary occurrence, helping men become more sensitive and nurturing and, thereby, better dads. Yet Fisch and others counter that fathers' declining testosterone levels aren't evolutionary but a result of the demands of child raising. "The lack of sleep, the lack of exercise, the belly starts showing up – it's that sedentary lifestyle."
While few doctors doubt that the more testosterone you take, the more muscle you build, some urologists, like Dr. Natan Bar-Chama of New York City's Mount Sinai Medical Center, question if more testosterone can also help other symptoms like depression, fatigue, and libido. "Are there physicians saying your numbers are low, testosterone could help?" asks Bar-Chama. "Yes. But are there also wellness centers giving people sesame oil and telling them it'll cure all diseases? Yes."
TRT has other side effects, too, including shrunken testicles, hair loss, acne, breast enlargement, and sterility. The therapy can also raise hematocrit levels (red blood cell concentration), which in turn can help improve athletic performance. But if your hematocrit level gets too high, the blood can become so viscous that it increases the risk of stroke and heart attack. “And what many patients don't realize”, says Bar-Chama, “is that testosterone is a lifelong therapy: Once you're on, your body stops making its own. Your brain sees the level is normal and shuts down."
That said, if you have classic symptoms of hypogonadism – low libido, fatigue, erectile dysfunction – "it's probably reasonable to check your testosterone. And for those guys whose blood levels come under definitions of low testosterone, it's probably reasonable to try the therapy for a while. But that's very different from saying testosterone is the fountain of youth."
Testosterone Replacement Therapy and Mortality in Older Men. Hackett 2016:
W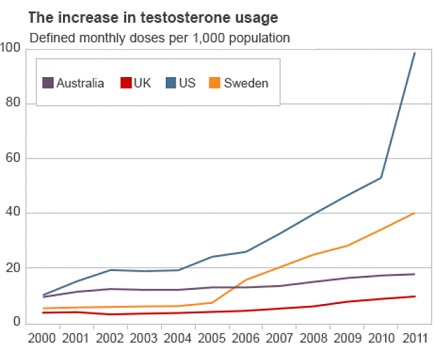 hile US testosterone prescriptions have tripled in the last decade with lower trends in Europe, debate continues over the risks, benefits and appropriate use of testosterone replacement therapy (TRT). Several authors blame advertising and the availability of more convenient formulations, whilst others have pointed out that the routine testing of men with erectile dysfunction (ED) (a significant marker of cardiovascular risk) and those with diabetes would inevitably increase the diagnosis of hypogonadism and lead to an increase in totally appropriate prescribing. They commented that this was merely an appropriate correction of previous under-diagnosis and under-treatment in line with evidence based guidelines. It is unlikely that persuasive advertising or convenient formulations could grow a market over such a sustained period if the treatment was not effective.
hile US testosterone prescriptions have tripled in the last decade with lower trends in Europe, debate continues over the risks, benefits and appropriate use of testosterone replacement therapy (TRT). Several authors blame advertising and the availability of more convenient formulations, whilst others have pointed out that the routine testing of men with erectile dysfunction (ED) (a significant marker of cardiovascular risk) and those with diabetes would inevitably increase the diagnosis of hypogonadism and lead to an increase in totally appropriate prescribing. They commented that this was merely an appropriate correction of previous under-diagnosis and under-treatment in line with evidence based guidelines. It is unlikely that persuasive advertising or convenient formulations could grow a market over such a sustained period if the treatment was not effective.
Urologists and primary care physicians are the most frequent initiators of TRT usually for ED. TRT is most frequently administered by intramuscular (im) injection of long-acting Testosterone esters or transdermally via patch or gel preparations and infrequently via oral administration. TRT produces a number of established benefits in hypogonadal men, including increased muscle mass, mood, cognitive function, strength, decreased fat mass, increased bone mineral density, and improved sexual function, and in some cases those benefits are dose dependent. For example, doses of TRT administered by im injection are typically higher than those administered transdermally, which results in greater musculoskeletal benefits.
There remains no evidence that TRT is associated with increased risk of prostate cancer or symptomatic benign prostatic hyperplasia, yet the decision to initiate and continue therapy is often decided by urologists. The cardiovascular issues associated with TRT have been clarified by recent studies showing that therapy associated with clear increases in serum testosterone levels to the normal range is associated with reduced all-cause mortality. Studies reporting to show increased risk have been subject to flawed designs with inadequate baseline diagnosis and follow-up testing. Effectively, they have compared non-treated patients with under-treated or non-compliant subjects involving a range of different therapy regimes. Recent evidence suggests long-acting injections may be associated with decreased cardiovascular risk, but the transdermal route may be associated with potentially relatively greater risk because of conversion to dihydrotestosterone by the effect of 5-alpha reductase in skin.
The multiple effects of TRT may add up to a considerable benefit to the patient that might be underestimated by the physician primarily concerned with his own specialty. In a response to concerns about the possible risks associated with inappropriate prescribing expressed by Public Citizen, the Food and Drug Administration (FDA) published a complete refutation of all the concerns, only to issue a subsequent bulletin of concern over inappropriate use, whilst confirming the benefits in treating men with established testosterone deficiency. No additional evidence was provided for this apparent change of opinion, but longer term safety data on testosterone products were strongly suggested. In contrast, the European Medicines Agency (EMA), in November 2014, concluded that “there is no consistent evidence of increased cardiovascular risk with testosterone products”. This paper explores the most recent evidence surrounding the benefits and risks associated with TRT.
B igPharma
igPharma
Testosterone is not just any drug. It’s not nitrous oxide out of a balloon at a Phish show or a little weed in a brownie. “T,” (as it is known) is, by most accounts, as close to a direct anti-aging medication as science has yet produced. It can be manufactured cheaply in large quantities, and the risks seem manageable for most people.
What we always predicted, the people that always demonized the bodybuilders and athletes that used anabolic androgenic steroids, are now selling testosterone and its analogues to whoever they can. Ironically? No, money talks.
Users on TRT report increased energy, more muscle mass, decreased body fat, greater sex drive, and a general sense of well-being. In short, it’s one of the most transformative substances a human can take.
“ Testosterone is ridiculously powerful,” Campion says. “I can tell you from experience, the feeling of well-being, of focus, and of masculine energy are massively increased. It’s like you’re back to being 35.”
Testosterone is ridiculously powerful,” Campion says. “I can tell you from experience, the feeling of well-being, of focus, and of masculine energy are massively increased. It’s like you’re back to being 35.”
That power — along with a heavy dose of pharma company marketing — is why millions of American men are obtaining testosterone from doctors in various forms. According to a study by University of Texas epidemiologist Jacques Baillargeon, nearly four percent of men in their 60s are taking testosterone. The number of men between 40 and 64 went up 77 percent from 2010 to 2013 to 1.5 million men.
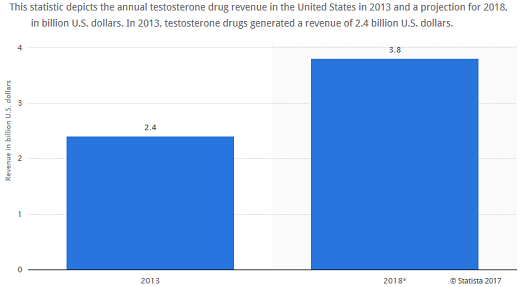
A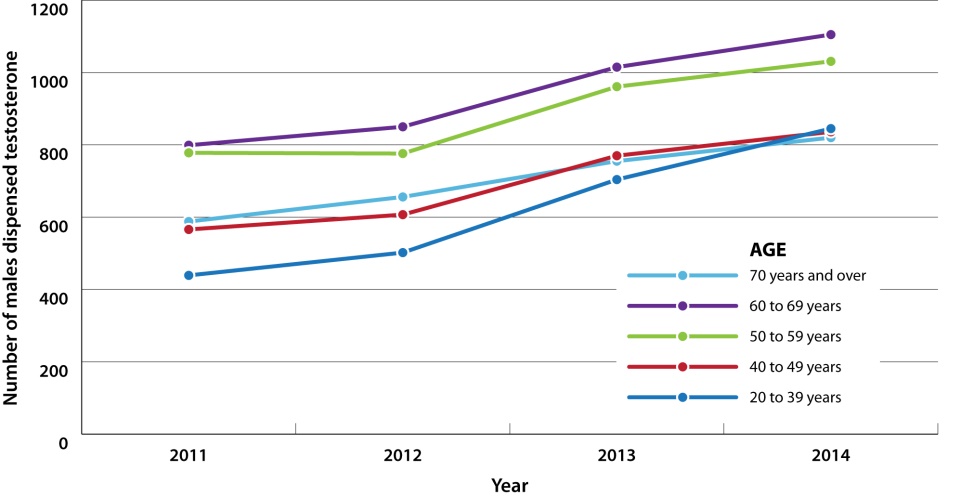 nd while ever-present ads like those from AbbVie Pharmaceuticals have buoyed sales of testosterone gels, that may be bad for patients as well as the United States’ $2.7 trillion annual health care bill.
nd while ever-present ads like those from AbbVie Pharmaceuticals have buoyed sales of testosterone gels, that may be bad for patients as well as the United States’ $2.7 trillion annual health care bill.
Sales of prescription testosterone gels that are absorbed through the skin generated over $2 billion in American sales in 2012, a number that is expected to more than double by 2017. Abbott Laboratories — which owned AbbVie until Jan. 1 — spent $80 million advertising AndroGel in 2012
In 2013, 14,000 kilograms of testosterone were sold in the United States. That might not sound like much, but a typical adult male has just 0.000000035 kilograms of testosterone floating around in his bloodstream. There is a lot of extra T in the hormonal composition of the country—and it only accounts for the legal sales.
Last year, drug makers in the United States spent $3.47 billion on advertising directly to consumers, according to FiercePharma.
 And America wouldn’t be America if attorneys wouldn’t try to get their slice of the cake, by suing AbbVie Pharmaceuticals etc.
And America wouldn’t be America if attorneys wouldn’t try to get their slice of the cake, by suing AbbVie Pharmaceuticals etc.
In March 2015, the FDA issued a safety warning that testosterone drugs may increase the risk of stroke, heart attack, and death in men taking FDA-approved testosterone products. Over 1,000 lawsuits filed by men who say testosterone drugs caused their cardiovascular problems are pending in federal court.



