Excess Estrogen
Most young men are dreading the day when their six-pack abs will bloat into a permanent beer belly, they will grow breasts and lose their libido.
Is it inevitable to look like this when you are middle-aged? Big Pharma would like us to believe that. But there is a lot you can do yourself to prevent such a body transformation.
Testosterone decline, which occurs naturally during age, was long thought to be sole reason for these middle-aged transformations. However, new evidence from Massachusetts General Hospital suggests estrogen – more commonly associated with female menopause – mediates some symptoms of “andropause” in men.

The idea of male menopause has solidified itself into medical culture in recent years, which has been matched by a tremendous boost in doctor’s prescriptions for testosterone supplements.
A 500 percent increase in prescriptions was recorded between 1993 and 2000, and this pattern continued over the course of the following decade.
This supplement boom occurred, despite the fact that it is not completely understood why testosterone deficiency causes physical symptoms – like muscle loss, weight gain, lowered sex drive, and fatigue – in middle-aged men.
Subcutaneous abdominal fat acts as a secretory gland, often producing and emitting excessive levels of estradiol into an aging man’s blood. One’s waist circumference is a highly accurate prognostic measurement of future disease risk, with excess estradiol secretion being at least one of the deadly mechanisms associated with the difficult-to-resolve problem of having too much abdominal fat.
Symptoms of excess estrogen in aging men include the development of breasts, having too much abdominal weight, feeling tired, suffering loss of muscle mass, and having emotional disturbances.
In 2013 at least 2.3 million testosterone prescriptions per year are written for men, and the use of testosterone in older men is expected to rise, given current trends.
In the course of the popularity of testosterone supplements in the U.S. market, the statistics of American males that received such testosterone medications have tripled and the replacement treatment has reached a point where it's almost $2 billion worth industry.
Male aging is accompanied by decreases in lean muscle mass and strength, bone mineral density, energy and sexual function. Increases in fat mass are also noted. Older men may be diagnosed with hypogonadism, and increasing numbers are being prescribed testosterone therapy. Research by Joel Finkelstein and colleagues at Massachusetts General Hospital provides a more detailed insight into the different roles of testosterone and estradiol in the body composition, strength and sexual function of men.
A new research led by Dr. Joel Finkelstein of Sunnybrook Research Institute attempts to distinguish the effects of estrogen and testosterone on male sexual performance, lean and fat mass, muscular size, and also to determine just the required levels of testosterones for health.
The research implies that the decreased levels of testosterone may mean a decline in strength, lean mass and muscular size. If there is no testosterone conversion to estrogen, this may mean body fat increase. And lack of both will trigger decreased sexual libido.
This study is important because it dissects the roles of both testosterone and estrogen in male body composition, strength and sexual function. Testosterone deficiency in men accounts for decreases in lean mass, muscle size, and strength, whereas estrogen deficiency primarily accounts for increases in body fat
The findings show that low testosterone levels triggers a decline in libido. But testosterone needs to fall significantly before sexual dysfunction affecting erection capability becomes noticeable.
The research implies that the decreased levels of testosterone may mean a decline in strength, lean mass and muscular size. If there is no testosterone conversion to estrogen, this may mean body fat increase. And lack of both will trigger decreased sexual libido. More on this study later in this blog-post.
Moreover, very low testosterone levels also result to decreased lean body mass strength in the legs and size of thigh muscles. Estrogen on its own doesn’t impact muscular size, leg strength or lean body mass. On the other hand, when production of estrogen is blocked, a rise in body fat results whatever the levels of testosterone is. Otherwise, a mild decrease of testosterone levels would cause body fat to increase
Serum testosterone levels gradually decline as men age,starting around age 35 to 40, but the degree to which this happens, as well as the extent of associated clinical changes, is variable. This age-related decline has been confirmed in several cross-sectional and longitudinal studies and results from dysfunction in the hypothalamic-pituitary-testicular axis. The clinical importance of this decline is controversial, however. Recognizing this variability and understanding what may be considered changes in body function due to "normal aging" versus potentially treatable age-related testosterone (or androgen) deficiency is crucial in the care of older men. The role of evaluating testosterone levels and their clinical significance is reviewed here.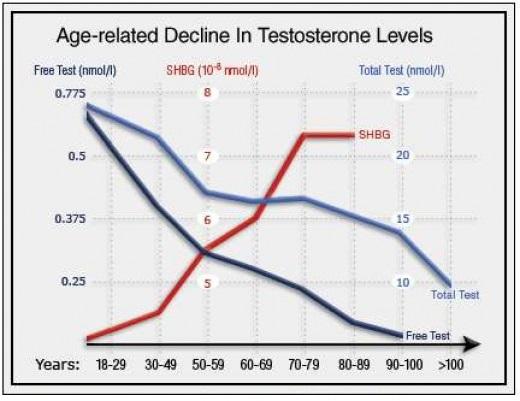
Aging is associated with declines in total serum testosterone concentration, increases in sex hormone-binding globulin (SHBG) concentration, and decreases in free testosterone. In one large cross-sectional study of more than 3000 men ages 40 to 79, serum testosterone concentration fell 0.4% per year, free testosterone concentration 1.3%. In another study, of 890 men, total testosterone levels were <325 ng/dL (considered androgen deficient) in 20%, 30%, and 50% of men in their 60s, 70s, and 80s, respectively.
Free testosterone is considered the biologically active form of the hormone. As men age, SHBG level rises, binding more testosterone and leaving less free testosterone available to act on target tissues. There is no uniformity in how aging men respond to this changing hormonal milieu, however. As a result, a controversy exists about whether this is a disease state. When it comes to low testosterone, what is normal senescence? What is illness?
Symptoms and signs suggestive of androgen deficiency in older men include reduced libido, low bone mineral density and height loss, and, less specifically, decreased energy, anemia, depressed mood, reduced muscle strength and bulk, and increased body fat. When these signs and symptoms accompany significantly lower levels of both types of testosterone, the patient may be diagnosed with late-onset hypogonadism. Cutoffs for the definition of low testosterone vary, although generally accepted values are ≤200 or ≤300 ng/dL of total testosterone.
Unlike younger men with hypogonadism who present prominently with specific gonadal dysfunction (for example, incomplete or delayed sexual development, infertility), older men have nonspecific symptoms that can frequently be caused by other common disorders. For example, in the largest longitudinal study of testosterone deficiency, researchers found that up to 25% of elderly men who complained of sexual dysfunction, including low libido and erectile dysfunction, had normal-range testosterone levels for their age. In light of these findings, what is the best approach to patients who may—or may not—need treatment?
The Endocrine Society updated its clinical guidelines on androgen deficiency evaluation and treatment in 2010. It proposed a practical approach to evaluating testosterone deficiency in older men who present with low libido, decreased energy, depressed mood, osteoporosis, or recent fracture. If a clinician suspects testosterone deficiency, the first step should include an early morning total testosterone measurement. If the level is <300 ng/dL, the test should be repeated twice to account for fluctuations. If levels remain below this threshold, the patient should be evaluated for pituitary or testicular disease. If these are ruled out, primary late-onset hypogonadism may be diagnosed and androgen treatment may be considered.
To date, there are relatively few well-designed, large studies on hypogonadism in aging men. To better understand if this is a distinct clinical syndrome, future trials should be powered to assess whether testosterone deficiency in older men independently predicts important outcomes such as osteoporosis, muscle strength, mood disorders, and sexual dysfunction. This will best inform us as we try to move forward with treatment. Obesity is strongly linked to low testosterone levels in men

Speaking of low libido, erectile dysfunction, gynecomastia and fat accumulation sounds familiar, right? It happens to many guys during or after cycling or after PCT. Some get so depressed and lethargic they lose the drive to go to the gym. The same sometimes also happens in the off season when guys party to long and eat and drink whatever they like. The principle of gaining fat – gaining more aromatase and thus gaining even more fat, is not restricted to old age.
It also happens to the younger gym-goer. And more and more to teens. It is due to a disrupted T/E ratio. This is not only due to estrogen conversion after testosterone administration but can also be caused by 'lifestyle' influences ( excessive alcohol, junkfood etc) which also affects levels of estrogen.
Obesity in men is associated with depressed levels of free and total testosterone and elevated levels of estradiol. In a vicious cycle, increasing abdominal obesity worsens hypogonadism, and without a compensatory gonadotropin response, hypogonadism worsens obesity. Worsening obesity is accompanied by increased aromatase activity in adipose tissue, rapidly converting testosterone to estradiol.
Low testosterone adversely affects overall health in many ways. Libido and sexual function are diminished, resulting in less sexual activity. Psychological effects of hypogonadism include depressed mood, decreased energy, and impaired cognition. Physical consequences are decreased bone density and higher risk of metabolic syndrome.
The potential impact of high estradiol on men’s health includes an increased risk of cardiovascular disease, including stroke and lower-extremity peripheral arterial disease (PAD). Abbott et al found that men in the highest quintile of estradiol concentrations face a significantly greater risk of stroke even after adjustment

This summary gives an overview of four research papers which discuss the link between obesity and low testosterone levels (also known as hypogonadism): one review focusing on the association between obesity, diabetes and low testosterone, and three clinical studies. The studies looked at the relationship between body mass index (BMI) and testosterone levels in men, and the effects of weight loss on testosterone levels in a group of very obese men (BMI >40 kg/m2) undergoing weight loss surgery; the link between obesity and testosterone levels in young men aged 14–20 years; and the relationship between health and lifestyle factors, including weight loss, and testosterone levels in men as they get older.
Key Findings
-
Obesity is a major cause of low testosterone levels
-
Hypogonadism is found in 75% of men considered very obese (BMI >40 kg/m2)
-
The link between obesity and low testosterone levels is found in men at all ages, even in young men and teenagers
-
The common decrease in testosterone seen in older men is not due to age, but rather to increasing body weight
-
Testosterone decreases seen in men as they get older can be reversed with weight loss
Age-associated changes in hypothalamic-pituitary-testicular function in middle-aged and older men are modified by weight change and lifestyle factors: longitudinal results from the European Male Ageing Study. Camacho EM, Huhtaniemi IT, O’Neill TW, et al. Eur J Endocrinol 2013;168(3):445-455.
Determinants of testosterone recovery after bariatric surgery: is it only a matter of reduction of body mass index? Luconi M, Samavat J, Seghieri G, et al. Fertil Steril 2013;99(7):1872-1879.
Testosterone concentrations in young pubertal and post-pubertal obese males. Mogri M, Dhindsa S, Quattrin T, et al. Clin Endocrinol (Oxf) 2013;78(4):593-599.
The role of obesity and type 2 diabetes mellitus in the development of male obesity-associated secondary hypogonadism. Saboor Aftab SA, Kumar S, Barber TM. Clin Endocrinol (Oxf) 2013;78(3):330-337.
Gonadal Steroids and Body Composition, Strength, and Sexual Function in Men.
Finkelstein et all 2013. This a very interesting study for us bodybuilders, since it shows the difference of dose response to testosterone against placebo and the concomitant use of Anastrozole a third-generation aromatase inhibitor.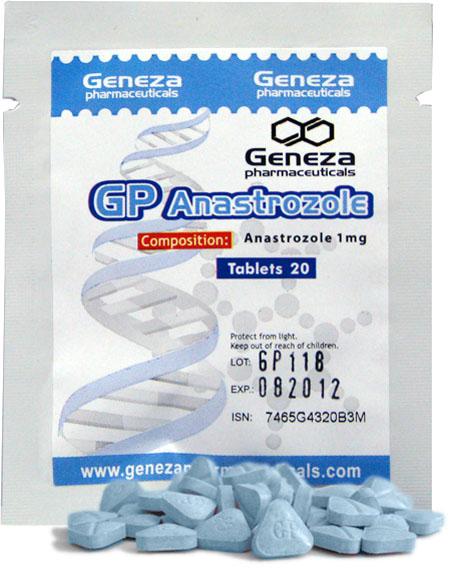
198 healthy men aged 20-50 years who were given goserelin acetate to suppress endogenous testosterone and estradiol. They randomized subjects to receive a placebo gel or 1.25, 2.5, 5, or 10 grams of testosterone gel daily for 16 weeks. 
Another 202 healthy men received goserelin acetate, placebo gel or testosterone gel, and anastrozole ( an aromatase inhibitor to suppress conversion of testosterone to estradiol).
More than 80% of circulating estradiol in men is derived from the conversion of testosterone, the investigators noted, so decreases in serum testosterone levels are accompanied by a decline in serum estradiol levels. “Nevertheless, the consequences of male hypogonadism are routinely attributed solely to androgen deficiency; the potential role of the concomitant decline in estrogens is typically ignored,” they observed.
In the men who did not receive anastrozole (cohort 1), the percentage of body fat increased significantly in those who received placebo or 1.25 or 2.5 grams of testosterone daily compared with subjects who received 5 grams of testosterone daily. 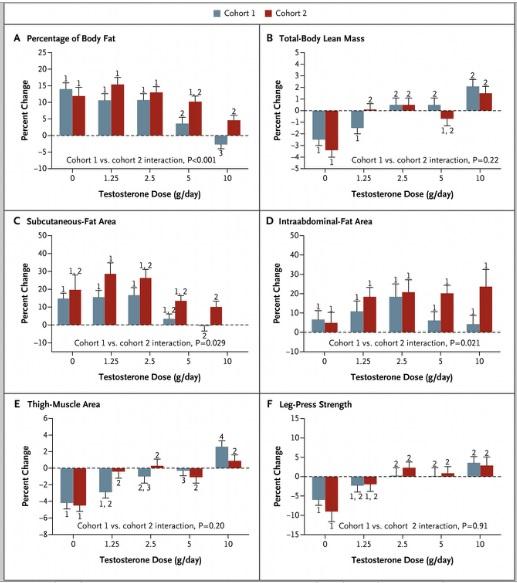
Lean mass declined significantly in men who received placebo or 1.25 grams of testosterone daily compared with men who received 2.5, 5, or 10 grams of testosterone daily.
Only placebo recipients experienced a decrease in leg-press strength.
In cohort 2, the percentage of body fat increased in all groups. The magnitudes of these increases were similar with placebo and 1.25, 5, and 5 grams of testosterone daily, a finding that suggests a predominantly estrogenic effect. Total-body lean mass decreased significantly in men who received placebo versus those who received 1.25, 2.5, and 10 grams of testosterone daily, “a finding that implies an independent effect of testosterone.” Subcutaneous-fat area increased in all groups in cohort 2, although only the comparison of changes between the 1.25 and 10 gram dose groups was significant.
Thigh-muscle area decreased significantly in men who received placebo compared with men who received any of the four testosterone doses, Dr. Finkelstein's group reported. Leg-press strength declined significantly in men who received placebo compared with those who received the three highest testosterone doses.
In cohort 1, sexual desire decreased progressively with declining testosterone doses. Erectile function worsened significantly in men who received placebo compared with men who received testosterone, and declined more in men who received 1.25 grams of testosterone daily than in those in the three highest dose groups.

In cohort 2, sexual desire declined significantly in men who received placebo compared with men in the three highest dose groups, and declined more in men who received 1.25 grams of testosterone daily than in subjects in the two highest dose groups. Erectile function decreased more in men who received placebo than in those who received testosterone.
“Our finding that estrogens have a fundamental role in the regulation of body fat and sexual function, coupled with evidence from prior studies of the crucial role of estrogen in bone metabolism, indicates that estrogen deficiency is largely responsible for some of the key consequences of male hypogonadism and suggest that measuring estradiol might be helpful in assessing the risk of sexual dysfunction, bone loss, or fat accumulation in men with hypogonadism,” the authors wrote.
Underground SERM’s and Aromatase Inhibitors (AI)
We have seen the difference an AI makes, when taking on a cycle. Many bodybuilders use SER’s like Nolvadex together with a third class AI. Many use underground supplements and underground made AI some as liquids, without making a statement I would like to post these analytical results.
However, bodybuilding discussion-forums have speculated that a dietary supplement called Esto Suppress contains tamoxifen because the label listed one of its chemical names . Four samples were purchased at different times between late 2011 and early 2012 and were analysed using reference standards and gaschromatography coupled with flame ionisation and mass spectrometry detectors. Tamoxifen was found in samples 1(3.8mg), 2(0.9mg), and 3(3.0mg), but not in sample 4. The product label suggested a dosage of two capsules a day, which in the case of sample 1 may have provided 7.6 mg of tamoxifen; 10-20 mg is used clinically for treating gynaecomastia. It is not known whether the Esto Suppress currently being sold still contains tamoxifen.
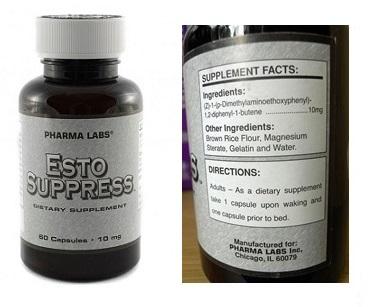
Esto Suppress containing tamoxifen. The label lists tamoxifen only by chemical name
(Z)-1-(p-dimethylaminoethoxyphenyl)-1,2-diphenyl-1-butene. The systematic name for tamoxifen is (Z)-2-(4-(1,2-diphenylbut-1-en-1-yl)phenoxy)-N,N-dimethylethan-1-amine



